Update from ..
But first to be excluded (2024-05-08) add to the below; developed in the last few weeks but now quite fast increasing = ALS-like symptoms (https://www.mayoclinic.org/diseases-conditions/amyotrophic-lateral-sclerosis/symptoms-causes/syc-20354022), including pulling and cramping in the arms, especially during the short periods of sleep. BUT most likely it is inflammation in the shoulders/arms related to a lot of use of crutches for several years! That is, chronic inflammation that probably decreases after I start using a walker!
… 2024-04-27 (my) main focus on …
Microbleeding in Pons has probably increased as hallucinations have increased significantly (see references below).
Now also visuospatial when I lie straight on my back or side but not when I sit. Like an extremely fast-paced movie (diffuse images) that I can’t stop where obscure ”people-like” fight (may have to do with the ”pre-memory” development of my PTSD during the first year in my life).
But it’s also likely what’s creating the hard-to-live ”alarm cluster” (back/brain stem = vice-like pain) from October 2019 after a head trauma accident. There is MRI 2020 & 2022 on microbleeds in the middle of Pons that are not taken into account despite my proposal for investigation. First now, neurologist Lauri Soinne, Medect.se, whom I met recently, had interesting comments on when microbleeds are in the middle of the pons! Will now try to get an investigation, but where in Sweden? Symptoms now increase even more during short sleep periods every night.
See also e.g.
Contributions of the Brainstem to the auditory and non-auditory components of Tinnitus
Part 1- The brainstem as a tinnitus generator
Part 2-The brainstem as a tinnitus modulator
Part 3-The brainstem’s role in tinnitus comorbidities”
https://www.ncrar.research.va.gov/Conference/Documents/PPT/Kaltenbach.pdf
Pons : Anatomy , Location & Function
https://anatomyinfo.com/pons-function/
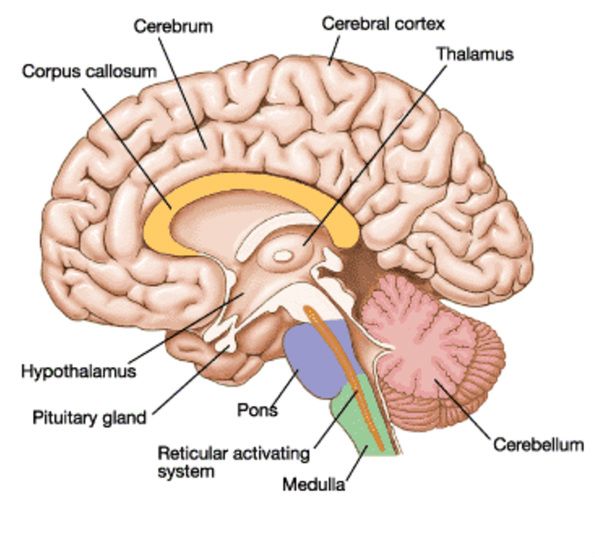 Pons: ”.. a portion of the brain lying inferior to the midbrain, above the medulla oblongata and anterior to the cerebellum. The pons is a broad, horseshoe-like shaped mass of transverse nerve fibers that connect between the cerebrum and cerebellum.
Pons: ”.. a portion of the brain lying inferior to the midbrain, above the medulla oblongata and anterior to the cerebellum. The pons is a broad, horseshoe-like shaped mass of transverse nerve fibers that connect between the cerebrum and cerebellum.
The pons measures roughly 2.5 centimeters (0.98 in) in length. The pons of the brainstem comprises neural pathways and tracts that conduct signals from the brain down to the cerebellum including medulla and tracts that transmit the sensory signals up into the thalamus.
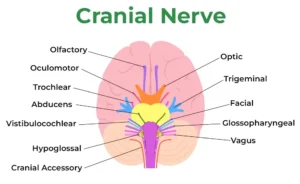
The pons comprises nuclei that carry signals from the forebrain through the cerebellum, along with nuclei that deal especially with sleep, respiration, bladder control, swallowing, hearing, equilibrium, taste, facial expressions, facial sensation, eye movement, and posture.
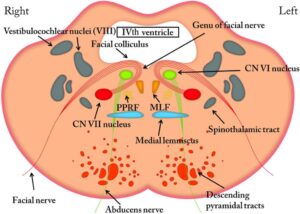
Pons ”hosts” e.g. Vestibucochear Nerve VIII
https://www.ncbi.nlm.nih.gov/books/NBK537359/figure/article-19673.image.f2/?report=objectonly
https://www.charlesbeaman.com/pons
More references
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3414436/<<
https://radiopaedia.org/articles/pontine-haemorrhage
https://pubmed.ncbi.nlm.nih.gov/37744632/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5411421/
(not) Latest news first
NBS the below is written with severe symptoms, hope readable
2024-03-30 (
a) The TMJ hypothesis can be downgraded due to careful examination + MRI (2024-01-21).
Remains
(b) (Until Barré-Lieout syndrome can also be hypothesized downgraded including that the nerves itself are inflamed cervical (and also or lumbar (head trauma accidental injuries C3-C7, L4-L5 and S1) not only via thermography (see also more text and picture at the botten)? and
(c) Neurologist Lauri Soinne, Medect AB, wrote to me on 2024.03-14 (first comment since 2018-04-26) about microbeeding in middle Pons: (see MRI below 2018-04-20) ”Localization in the middle of the pons is interesting – from the pons you can get even auditory hallucinosis”.
”Auditory hallucinations, or paracusias, are sensory perceptions of hearing in the absence of an external stimulus. Auditory hallucinations can refer to a plethora of sounds; however, when the hallucinations are voices, they are distinguished as auditory verbal hallucinations.” https://www.ncbi.nlm.nih.gov/books/NBK557633/
* BUT a Pons dysfunction can also increase risks of ”small vessel disease” or ”amyloidosis” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9860402/ (The paradigm of amyloid precursor protein in amyotrophic lateral sclerosis: The potential role of the 682YENPTY687 motif) ”Neurodegenerative diseases are characterized by the progressive decline of neuronal function in several brain areas, and are always associated with cognitive, psychiatric, or motor deficits due to the atrophy of certain neuronal populations.
Most neurodegenerative diseases share common pathological mechanisms, such as neurotoxic protein misfolding, oxidative stress, and impairment of autophagy machinery.
Amyotrophic lateral sclerosis (ALS) is one of the most common adult-onset motor neuron disorders worldwide. It is clinically characterized by the selective and progressive loss of motor neurons in the motor cortex, brain stem, and spinal cord, ultimately leading to muscle atrophy and rapidly progressive paralysis.
Multiple recent studies have indicated that the amyloid precursor protein (APP) and its proteolytic fragments are not only drivers of Alzheimer’s disease (AD) but also one of the earliest signatures in ALS, preceding or anticipating neuromuscular junction instability and denervation. Indeed, altered levels of APP peptides have been found in the brain, muscles, skin, and cerebrospinal fluid of ALS patients
2018-04-26 MRI = ”Isolated punctate changes in subcortical and deep white matter and a pointy* hemosideriemise in the centre of the pons, all of a microangiopathic nature in the first place” (Hemosiderin? = deposits of insoluble iron in the body that can cause organ damage + Microangiopathy — i.e. an infarction/embolism in one of the small vessels that go to the nerve is a common cause. Microangiopathy, in turn, is usually caused by diabetes mellitus, hypertension and/or atherosclerosis”)
https://www.internetmedicin.se/behandlingsoversikter/ogon/abducenspares-n-vi/#:~:text=Mikroangiopati%20%E2%80%94%20d%20v%20s%20en%20infarkt%2Femboli,%2C%20hypertoni%20och%2Feller%20ateroskleros.
> https://radiopaedia.org/articles/subarachnoid-haemorrhage + https://pubmed.ncbi.nlm.nih.gov/23832987/#:~:text=Hemosiderin%20deposition%20is%20the%20consequence,with%20diffuse%20and%20symmetrical%20margins. + https://tidsskriftet.no/en/2017/08/medisinen-i-bilder/cerebral-hemosiderin-deposition + https://en.wikipedia.org/wiki/Central_pontine_myelinolysis#:~:text=Central%20pontine%20myelinolysis%20is%20a,an%20area%20of%20the%20brainstem).
Brain haemosiderin in older people: pathological evidence for an ischaemic origin of magnetic resonance imaging (MRI) microbleeds https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4282337/
Working on the above -> More is t come here but I move right now to
Locus Coeruleus
NB LC = Locus Coeruleus – Link coming
The problem with the above micro bleed in the middle of Pons is that Locus Coeruleus (and NE) are complicating direct and also indirect – including most dysfunctions …
“.. The locus coeruleus has widespread norepinephrine projections throughout the central nervous system, which act to globally modulate arousal states and adaptive behavior, crucially positioned to play a significant role in modulating both ascending visceral and descending cortical neurocognitive information ..” BvS and more … https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7479871/
“The study provides evidence that older adults had reduced functional connectivity between the LC and SN (Silent Network) compared with younger adults, evidenced by increased coupling of the CEN network to the SN than the DMN. These authors conclude that the reduced interactions between the LC and SN impair the ability to prioritize the importance of incoming events. In turn, the SN fails to initiate network switching (4, 176), which would promote further attentional processing (266). The continued study of open access data sets using computational tools such as multivariate analysis will increase the amount of information decoded from brain activity (267). In particular, the LC will be a fascinating subject of study over varied timescales and sub-regions, as it likely mediates the vast array of behavioral and physiological outputs by coding responses differentially over short and long timescales. A number of disorders arise from hyper-activation of the SN that directly or indirectly relates to dysfunction of the LC-NE system. Among them, a convincing case can be made for post-traumatic stress disorder and opiate use disorder, in which the aberrant assignment of high salience to trauma- or drug- experience related stimuli hinder patient progress to recovery”
Also GABA as the main inhibitor of excitatory neurotransmitters as NE ((see also https://www.boaim2.se/innovativm2/gaba-and-more/ and sub pages) play an important role also in this case!
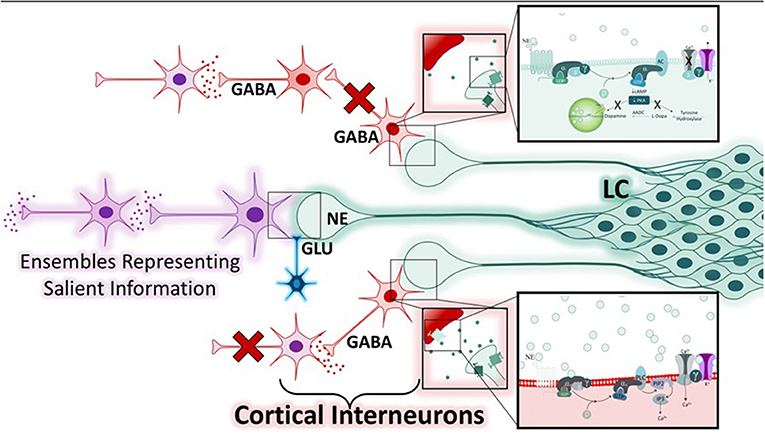
https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2020.601519/full
AS my GABA is low, this in turn increase complexity of LC/NE influence also in Pons and Reticular Activation System and thereby also arousal.
Arousal and RAS
« Arousal may be understood on a spectrum, with excessive sleepiness, cognitive dysfunction, and inattention on one side, a wakeful state in the middle, and hypervigilance, panic, and psychosis on the other side. However, historically, the concepts of arousal and stress have been challenging to define as measurable experimental variables. Divergent efforts to study these subjects have given rise to several disciplines, including neurobiology, neuroendocrinology, and cognitive neuroscience. We discuss technological advancements that chronologically led to our current understanding of the arousal system, focusing on the multifaceted nucleus locus coeruleus. We share our contemporary perspective and the hypotheses of others in the context of our current technological capabilities and future developments that will be required to move forward in this area of research.
See also https://www.boaim2.se/issues/arousal-definition-and-applications-mostly-of-clinical-concern/
Why no habituation in the main symptom but otherwise perfect habituation?
2024-08-06 Our knowledge here is very limited but about is not functional, although 5 years of permanent of high levels of symptoms indicate that RAS ”is specifically out of order” any king of adaptions occurs! One possibility is that in this special case (quantum associated, speculative!) enzymatic inefficacy prevent proper habituation in RAS. But this does not explain while habitation occur in other stimuli! Or that the symptom stimulus generation is too fast overriding the orienting – and or startle response – sounds not possible?
Example of history: In August 2021 I wrote which will be updated and moved to cervikal dysfunctions and … see also https://carism.se/2023-2/cervicocranial-syndromes-including-barre-lieou-syntrome-neck-pain-blurred-vision-nausea-vertigo-tinnitus-tmj/
Since October 2019 I suffer from, very complex, hard to stand, sound/pain symptoms probably associated with head trauma 2018 where spinal dysfunctions (MRI data 2020-02-07) have been probably further developed (degeneration/spondylitis/foraminala stenosis.. preferably cervikal and lumbar in complex interactions) causing multifaceted ”close” (non-dynamic permanent activated since it started October 2019) systems interplay also influencing sympathetic nervous system (SNS) both local (spinal instability/dysfunctions influencing vertebrobasilar vascular processes – see two pictures below) and in general possibly also influencing Locus Coeruleus causing further complex symptoms
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5691173/,
How cervical spine instability disrupts blood flow into the brain and causes many neurological problems – Caring Medical Florida (the picture below)
https://www.caringmedical.com/prolotherapy-news/vertebrobasilar-insufficiency/
” What are we seeing in this image? The cervical spine is intertwined with nerves and blood vessels. Cervical spine instability can compress or pinch the nerves and arteries causing a myriad of symptoms depending on how the patient moves his/her head. Cervical spine instability can cause restriction and compression of vital arteries and nerves that supply blood and sensation to the brain, face, and neck.”
BvS comment: What we do SEE (visualize) is the complexity but we hardly SEE (understand) complex integrating systems ”expressions” in general as well as in (what counts in clinical work) particular – something needed to be more addressed in empirical studies AND clinical work – at individual levels, e.g. using single case designs!
– And
For myself (as a patient) to following the above hypothesis diagnosis, focus on to increase modifying and tailoring of our biopsychosocial medicine toolbox – but where more objective outcome (dependent measure) measures still is lacking in present knowledge (As I know of) motivating so far only to use symptoms as dependent variable/outcome measure.
And the link above goes on: “In our clinic’s research published in The Open Orthopaedics Journal (8), we wrote that the capsular ligaments are the main stabilizing structures of the facet joints in the cervical spine and have been implicated as a major source of chronic neck pain. Such pain often reflects a state of instability in the cervical spine and is a symptom common to a number of conditions such as disc herniation, cervical spondylosis, whiplash injury, and whiplash-associated disorder, post-concussion syndrome, vertebrobasilar insufficiency, and cervicocranial syndrome. When the capsular ligaments are injured, they become elongated and exhibit laxity, which causes excessive movement of the cervical vertebrae. In the upper cervical spine (C0-C2), this can cause symptoms such as nerve irritation and vertebrobasilar insufficiency with associated vertigo, tinnitus, dizziness, facial pain, arm pain, and migraine headaches.
More detailed personal (patient) text: After more than 1.5 years of – extremely difficult to live with (but still I do knowing other also suffer and lack of knowledge is urgent needed, which I focus on) – permanent blasting & occasional high-frequency cutting sounds (both in head/neck) & pain symptoms* in the head, neck, thoracic spine and lumbar spine, I have long been aware that my spinal stenoses/spondyloses after head trauma**, where a destructive further development occurs, likely resulting in very difficult symptomatic symptoms, one of which is permanent until now since October 2019
In passivity/rest and sleep, sound/pain symptoms (may relate to associated metabolic dysfunction, possibly also including hypoxia) increase where, where oddly enough, my dreams during sleep ”develop” from irrational, destructive content to more and more constructive, positive dreams – even though the symptoms did not decrease, but increased slightly in the last few months, with ”seizure-like” reactions*** (I do not refer to Exploding Head Syndrom, which I have had for years) when I sleep more than 2-3 hours at a time**** – but in all sleep is enough independent of symptoms increases.
May add that I have had well-manageable 60-year-old noise-affected tinnitus, which makes me increasingly realize that my current difficult problems (where my noise-affected tinnitus is probably left masked by the ”alarm”) do NOT fit in with how one apparently usually ”sees” (without detailed biopsychosocial investigations – http://carism.se/projekt-carism/urgent-needed-knowledge-and-practice-development-different-kinds-of-tinnitus/ and www.biopsychosocialmedicine.com) the tinnitus syndrome, at least in Sweden
My intervention biopsychosocial toolbox (based on my dissertation 1986, and gradually refined during the years) is discussed elsewhere.
MRI 2020-02-07 shows cervical and lumbar foraminal stenosis mainly right due to pronounced facet joint arthritis and a sized herniated disk C5-C6 with light influence on medulla. As well as problems with broad-based disc herniation dura sack effect just over the limit of spinal stenosis L3-L4 simultaneously left-sided lateral recess stenosis L4-L5 with possible L5 root influence and left-sided herniated disk L5-S1
Also – not-airborne sinus Maxillaries could be associated with hypoxia with related clinical complications – may be a part of the symptoms associated with pressure change sensitivity? Some additional findings is coming here.
* One symptom I have not mentioned above is visual disturbances (possibly such as silent migraines) that indicate that the optic nerve is also affected – however, this occurs temporarily for as yet unidentified causes. Another is refluxes possibly associated with cervical enervation of Sympatric (see below) nerves which in turn influence (lower) esophageal sphincter
** Handless with my head into a concrete pillar in Helsinki 2018 where I was for the treatment of aggressive prostate cancer, on my way to the airport)
*** May relate to overreaction – related to constant imbalance due to cervical instability, see below, especially the picture – at restarting the sympathetic nervous system after REM sleep (ref). However, in daytime psychophysiological measurements (usually not assumed SNS ”seizures”), autonomic nervous system (ANS) oscillation is normal as clearly visible in the Respiratory Sinus Arrhythmia Pattern (RSA is not a clinical arrhythmia but an indication of biological central normal oscillatory process related to the ins and excrement.
**** Something that may be attributable to hypnotic experiments I work with (only myself as a subject until further notice, even before the above severe symptoms). Something that might (!!) eventually have a psychological/limbic reciprocal effect on biological dysfunction via psychological placebo influence – overtime? As a researcher, I do not want to limit myself creatively and innovatively, well aware that it is far from the ”mainstream”, which unfortunately (accidentally?) can scare sometimes (?) to ”reductionistic simplicity”