The below can be regarded as a personal documentation out of a clinical perspective in a field new to me, which I now by personal reason try to learn/understand/work with … to get well! Unfortunately, Unfortunately, tinnitus, based on no real investigated diagnosis hypothesis, was very wrong and misleading during more than one year, while the below more plausible!
NB, a warning, my dyslexia can enable misunderstanding? – see also 2021 links on cervical instability – on Mostly fragmentary links on different perspective on the Tinnitus Syndromes | CARISM – Complex Auditory Related Integrated Systems Medicine
Also – this page is growing and content much more below than ”My actual diagnosis hypothesis”, with some of it, for me, new interesting pictures/texts e.g. ”clarifying …”
Before reading ”Last brief ..” and ”My actual ..”, I will emphasize three links discuss below while especially important as I see it; https://pubmed.ncbi.nlm.nih.gov/24892904/ – https://pubmed.ncbi.nlm.nih.gov/24892904/ – https://www.physio-pedia.com/Tinnitus and https://www.caringmedical.com/prolotherapy-news/tinnitus/
Very brief last updated 2021-12-26
Will write more when I have considered how to explain what I have done (quite much from my toolbox) as well as what is addressed as dysfunctional (without proper multidisciplinary test absent) but right now: Main focus in on complex Osteomeatal complex behaviors and its interactions where (a) dishabituation (of the permanent so far -> “alarm”), RAS and Locus Coeruleus (especially overactivation after REM-sleep rest) and associated Limbic operational conditionings increase the complexity. My self-interventions (based on my biopsychosocial toolbox – dissertation 1986) is quite complex developed during the years but will be in detail described when (i) single case outcome documentation is sufficient and (b) time permit at http://carism.se/2021-2/brief-overview-and-summarizing-my-personal-fight-against-impossible-blasting-head-symptoms/
Not latest brief updates 2021-10-06
Actual priority (more of an overview below ”2021-09-27)
(a) Investigate what cause increased ”alarm” during night sleep, each nigh for 2 years? It increases more at 2 hours of sleep than of 1. Possibly not well aerated cavity (related to head trauma) = increased local hypoxia/tension/pressure during inactivity. When I manage to mitigate with motion programs a little, at the same time internal gas reactions with flatulence also occur. Variations in air pressure affect 24 hours constant head blasting sound-pain – sometimes similar in effects as during sleep. The negative development can also be associated with increased myelitis (https://www.mayoclinic.org/diseases-conditions/transverse-myelitis/diagnosis-treatment/drc-20354730) degeneration?
(b) Increased lumbar problems including hip problems and for the first time (often) increased problems to walk. Previously had osteoarthritis in the knees (both ”new”, cleaned” knee joints) and feet
(c) Observed strange association between eye problems (ophthalmologists do not find eye problems but well migraine-typical symptoms – silent migraine?) and nose-related problems (incl. osteomeatal complex?) while having ”tricky” symptoms such as I had earlier = complex sinusitis. https://www.bergerhenryent.com/your-sinus-headache-could-actually-be-a-migraine-headache/
2021-09-27
Physiological symptoms: permanently blasting sound-pain ”alarms” including no habituation (!) that gets worse, which after 2 years (when it started) is clearly negatively developing. Probably due to head/spinal trauma (accident) where possibly some not well aired cavity, including hypoxia & pressure variations & micro function. Possibly even via excess excitatory neurotransmitters´ via outer hair cells influencing my 60-year-old old (manageable too loud music related) tinnitus, which than can substantially increase. The negative development may also be associated with increased myelitis* degeneration. Increased severity to walk may refers to hip osteoarthritis (have had many years arthritis in knee and foot.
During sleep the symptoms becomes temporary even worse (increase more for each slept hour) and also by air pressure changes as well. But can be reduced to pre stimuli level with strategy programs.
Psychologically-emotional state: Am feeling surprisingly good despite (see above) hard biological symptoms.
For me, it is important to investigate furthermore physiological possible causes of the symptoms because the dysfunction(s) seem to be degenerate over time.
* An additional (actually ”new-old”) trace is emerging, to be excluded = “Transverse myelitis” associated with my head trauma and probably degenerating spinal dysfunctions
https://www.mayoclinic.org/diseases-conditions/transverse-myelitis/diagnosis-treatment/drc-20354730.
2021-08-22
(symptoms explanation more below)
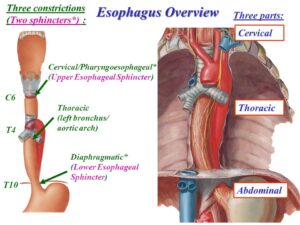
After unusual long sleep period, 4 hours (a) GERD (lower esophageal sphincter dysfunction – heart burn) increased substantially but (b) increase of permanent head blasting was “normal” since 1,5 y assumed associated with spinal dysfunction, which is new while a long period of sleep earlier did increase dependent on sleep period time – which I interpret as promising … also selfcare strategies recovery was shorter in time as well as more effective. Probably is enervation of local (and the general) sympathetic system united reason for this – motivating predicted self-care exercise
Beginning to learning to (limbic) ignore the symptom alarms, although I do not get much help from the evolution and orienting response/dishabituation as well as activated Locus Coeruleus behaviors …
My actual (July-August) diagnosis hypothesis:
Abstract:
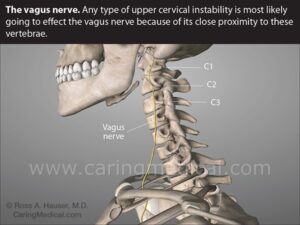
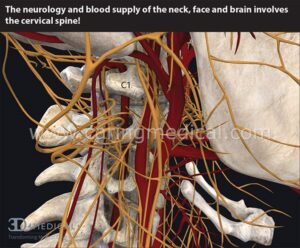
Since October 2019 I suffer from, very complex, hard to stand, sound/pain symptoms probably associated with head trauma 2018 where spinal dysfunctions (MRI data 2020-02-07) have been probably further developed (degeneration/spondylitis/foraminala stenosis.. preferably cervical and lumbar in complex interactions) causing multifaceted ”close” (non-dynamic permanent activated since it started October 2019) systems interplay also influencing sympathetic nervous system (SNS) both local (spinal instability/dysfunctions influencing vertebrobasilar vascular processes – see two pictures below) and in general possibly also influencing Locus Coeruleus causing further complex symptoms
(https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5691173/, How cervical spine instability disrupts blood flow into the brain and causes many neurological problems – Caring Medical Florida (the picture below)
 https://www.caringmedical.com/prolotherapy-news/vertebrobasilar-insufficiency/
https://www.caringmedical.com/prolotherapy-news/vertebrobasilar-insufficiency/
” What are we seeing in this image? The cervical spine is intertwined with nerves and blood vessels. Cervical spine instability can compress or pinch the nerves and arteries causing a myriad of symptoms depending on how the patient moves his/her head. Cervical spine instability can cause restriction and compression of vital arteries and nerves that supply blood and sensation to the brain, face, and neck.”
BvS comment: What we do SEE (visualize) is the complexity but we hardly SEE (understand) complex integrating systems ”expressions” in general as well as in (what counts in clinical work) particular – something needed to be more addressed in empirical studies AND clinical work – at individual levels, e.g. using single case designs!
– And
For myself (as a patient) to following the above hypothesis diagnosis, focus on to increase modifying and tailoring of our biopsychosocial medicine toolbox – but where more objective outcome (dependent measure) measures still is lacking in present knowledge (as I know of) motivating so far only to use symptoms as dependent variable/outcome measure.
And the link above goes on: “In our clinic’s research published in The Open Orthopaedics Journal (8), we wrote that the capsular ligaments are the main stabilizing structures of the facet joints in the cervical spine and have been implicated as a major source of chronic neck pain. Such pain often reflects a state of instability in the cervical spine and is a symptom common to a number of conditions such as disc herniation, cervical spondylosis, whiplash injury, and whiplash-associated disorder, post-concussion syndrome, vertebrobasilar insufficiency, and cervicocranial syndrome. When the capsular ligaments are injured, they become elongated and exhibit laxity, which causes excessive movement of the cervical vertebrae. In the upper cervical spine (C0-C2), this can cause symptoms such as nerve irritation and vertebrobasilar insufficiency with associated vertigo, tinnitus, dizziness, facial pain, arm pain, and migraine headaches.
More detailed personal (patient) text: After more than 1.5 years of – extremely difficult to live with (but still I do knowing other also suffer and lack of knowledge is urgent needed, which I focus on) – permanent blasting & occasional high-frequency cutting sounds (both in head/neck) & pain symptoms* in the head, neck, thoracic spine and lumbar spine, I have long been aware that my spinal stenoses/spondyloses after head trauma**, where a destructive further development occurs, likely resulting in very difficult symptomatic symptoms, one of which is permanent until now since October 2019
In passivity/rest and sleep, sound/pain symptoms (may relate to associated metabolic dysfunction, possibly also including hypoxia) increase where, where oddly enough, my dreams during sleep ”develop” from irrational, destructive content to more and more constructive, positive dreams – even though the symptoms did not decrease, but increased slightly in the last few months, with ”seizure-like” reactions*** (I do not refer to Exploding Head Syndrom, which I have had for years) when I sleep more than 2-3 hours at a time**** – but in all sleep is enough independent of symptoms increases.
May add that I have had well-manageable 60-year-old noise-affected tinnitus, which makes me increasingly realize that my current difficult problems (where my noise-affected tinnitus is probably left masked by the ”alarm”) do NOT fit in with how one apparently usually ”sees” (without detailed biopsychosocial investigations – http://carism.se/projekt-carism/urgent-needed-knowledge-and-practice-development-different-kinds-of-tinnitus/ and www.biopsychosocialmedicine.com) the tinnitus syndrome, at least in Sweden
My intervention biopsychosocial toolbox (based on my dissertation 1986, and gradually refined during the years) is discussed elsewhere.
MRI 2020-02-07 shows cervical and lumbar foraminal stenosis mainly right due to pronounced facet joint arthritis and a sized herniated disk C5-C6 with light influence on medulla. As well as problems with broad-based disc herniation dura sack effect just over the limit of spinal stenosis L3-L4 simultaneously left-sided lateral recess stenosis L4-L5 with possible L5 root influence and left-sided herniated disk L5-S1
Also – not-airborne sinus Maxillaries could be associated with hypoxia with related clinical complications – may be a part of the symptoms associated with pressure change sensitivity? Some additional findings is coming here.
* One symptom I have not mentioned above is visual disturbances (possibly such as silent migraines) that indicate that the optic nerve is also affected – however, this occurs temporarily for as yet unidentified causes. Another is refluxes possibly associated with cervikal enervation of Sympathic (see below) nerves which in turn influence (lower) esophageal sphincter
** Handless with my head into a concrete pillar in Helsinki 2018 where I was for the treatment of aggressive prostate cancer, on my way to the airport)
*** May relate to overreaction – related to constant imbalance due to cervical instability, see below, especially the picture – at restarting the sympathetic nervous system after REM sleep (ref). However, in daytime psychophysiological measurements (usually not assumed SNS ”seizures”), autonomic nervous system (ANS) oscillation is normal as clearly visible in the Respiratory Sinus Arrhythmia Pattern (RSA is not a clinical arrhythmia but an indication of biological central normal oscillatory process related to the ins and excrement.
**** Something that may be attributable to hypnotic experiments I work with (only myself as a subject until further notice, even before the above severe symptoms). Something that might (!!) eventually have a psychological/limbic reciprocal effect on biological dysfunction via psychological placebo influence – overtime? As a researcher, I do not want to limit myself creatively and innovatively, well aware that it is far from the ”mainstream”, which unfortunately (accidentally?) can scare sometimes (?) to ”reductionistic simplicity”
More reasoning text: See also the picture below (https://www.pinterest.se/pin/68328119332011100/) is one (of several) starting points(s) where chronic local enervation of sympathetic effects has many effects, including vasoconstriction that directly and/or indirectly (has several local suggestions, but I am still waiting for some kind of investigative indications, see example below) which explains why no habituation occurs and probably even permanent dishabituation occurs possibly also affecting the reticular activation system and Locus Coeruleus (which I work with in my doctoral dissertation 1986).
There are more symptoms temporarily that are likely to constitute ”further developments” from above where probably also local hypoxia is included, there are many different ”places” it may have occurred and that have been further developed after the head trauma initiation. Increased reflux problems can also be linked to the influence of sympathy on sphincter (muscle) functions…
Discuss more below cervical instability (about which there are very different perceptions of … – see also http://carism.se/projekt-carism/a-multidisciplinary-overview-of-the-tinnitus-syndrome-fields/overview-of-some-of-the-tinnitus-syndrome-approaches/)
Cervical Instability: Causes, Symptoms, & Treatments
https://denveruppercervical.com/cervical-instability/
— symptom… many e.g. muscle spasms, neck, shoulder or jaw pain, difficulty swallowing, sensitivity to light, blurred vision, tinnitus, vertigo ..
Diagnose cervical instability
How to test cervical instability? Here are 4 test methods for cervical instability:
- Upright MRI (AKA magnetic resonance imaging)
2. Supine MRI (lying on the back)
3. CT scan (AKA computerised CT scan)
4. Digital X-ray
It’s worth mentioning that although MRI is the most common diagnostic test method for cervical instability, a 2012 scientific study found that MRI had limited diagnostic value in patients with whiplash-associated diseases” such as cervical instability.
Here are some measurements to diagnose cervical instability:
- Clivo-Axial Angle less than or equal to 135 degrees (https://me-pedia.org/wiki/Clivo-axial_angle)
- Grabb-Oakes measurement greater than or equal to 9 mm (https://me-pedia.org/wiki/Craniocervical_instability)
- Harris measurement greater than 12mm (https://radiopaedia.org/articles/atlanto-occipital-dissociation-injuries)
- Possible spinal subluxation (https://tuckclinic.com/blog/2020/10/01/what-is-a-spinal-subluxation/)
Some more links:
https://me-pedia.org/wiki/Basilar_invagination
https://link.springer.com/article/10.1007/s00586-017-5360-8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7695767/ https://www.ncbi.nlm.nih.gov/books/NBK539753/ https://immunityageing.biomedcentral.com/articles/10.1186/s12979-020-00177-x https://www.researchgate.net/publication/350770516_Subclinical_infection_can_be_an_initiator_of_inflammaging_leading_to_degenerative_disk_disease_evidence_from_host-defense_response_mechanisms https://www.frontiersin.org/articles/10.3389/fimmu.2020.622772/full https://www.uofmhealth.org/health-library/abr8401#:~:text=Spondylosis%20is%20age%2Drelated%20change,range%20from%20mild%20to%20severe
https://www.caringmedical.com/prolotherapy-news/craniocervical-instability/ https://pubmed.ncbi.nlm.nih.gov/33082920/
https://www.physio-pedia.com/Sharp_Purser_Test
https://www.caringmedical.com/prolotherapy-news/gerd-neck/
https://www.caringmedical.com/prolotherapy-news/neck-problems-cause-urinary-incontinence/
https://www.healthline.com/human-body-maps/vagus-nerve
https://www.wikihow.com/Diagnose-Vagus-Nerve-Damage
Looks like chiropractic, especially internationally, developed comprehensive diagnostic tools
https://www.pinterest.se/pin/68328119332011100/
(BvS) Hypothesis Diagnoses Reasoning: Above image ”Vertebrae shoot …” motivation including local sympathetic nervous system (SNS) dysfunctional activity and which Refluxes (mostly silent but sometimes very typical symptoms) can also behave dysfunctional due to not functional SNS and because refluxes for many years are part of my own ”symptom picture” cervical instability can interact / affect Pharyngo esophageal function (esophageal sphincter function ) because the sphincter function ”reversed” = increased SNS increase reduces the esophageal sphincter muscles and works = facilitates reflux behavior – a lot of info on the https://www.ncbi.nlm.nih.gov/books/NBK557452/ see also below image
https://slideplayer.com/slide/7891920/
More reasoning based on my own experiences from actual patient position; ”While people may experience GERD (gastro-esophageal reflux disease) and back pain at the same time, gerd is more likely to be caused by something related to the existing back pain or its treatment, rather than GERD that causes back pain. Here are some possible causes of GERD and acid reflux related to back pain – and how to deal with them,” https://www.spine-health.com/blog/can-gerd-cause-back-pain
But also, quiet refluxes and refluxes via ”Reciprocal Causal Relationship between Laryngopharyngeal Reflux and Eustachian Tube Obstruction” http://medcraveonline.com/JOENTR/JOENTR-02-00046.pdf is not to be forgotten.
A symptom change (increased) observation can provide diagnoses hypotheses reasoning material? It is during the nights (the last 20 years I sleep 8-10 h excellently) but after the severe permanent rupture symptoms arose (October 2019) a pronounced increase developed, always in the last 2-3 hours, together (in parallel) with increased back pain (lumbal?) pain (has MRI data on L4-L5 foraminal stenoses and S1 herniated disks) and a two-point neck (moderate) pain. Interaction between ???
Also strange that reflux symptoms develop during exercise cycling but not during treadmill exercise
In addition; About refluxes and tinnitus – https://www.betterbalanceinlife.com/the-gut-and-vertigo/ ”If you have acid reflux (or heartburn) and dizziness, I think this article might be interesting to you…. I think the author presents a very interesting idea that the ”reflux material” can exacerbate the Eustachian tubes that go from the middle ear to the neck.
I have had patients with vertigo episodes related to acid reflux.
This association is called ”sur labyrinthitis” and can result in tinnitus, dizziness and vertigo.
The re-infested food particles and stomach acids can irritate the ear, although the eustachian tube that connects the throat to the ear.
Esophageal inflammation, or inflammation of the esophagus, is often involved due to throat irritation as well”. .. Suddenly in December, he had acid reflux. I had never had it before in my life, never woke up with tonsils/sinus/nose etc which may have made me suspect a silent reflux..
… … I went to a gastroenterologist doctor, who basically just looked at me like I was crazy and laughed at me for asking if I was dizzy because of acid reflux!!! Dr Bell replies above: You may have silent reflux and/or esophageal inflammation….”
Summarizing; Cervical instability and silent refluxes can cause a number of symptoms where I focus on what are most symptoms driven by hypotheses diagnostic reasoning. Since clinical investigations are complex and cannot always clearly identify without different assessment methods, I use psychophysiological tools from the toolbox that – given the above reasoning is wrong – do not harm but are instead part of my health promotion activities I enjoy!
Synopsis; Knowledge development around the intestinal-brain axis really justifies open mind of system interactions, especially we will probably more generally increase our underhalation of omplex biopsycosocial medicine interaction (www.biopsychosocialmedicine.com)
More clarifying below?
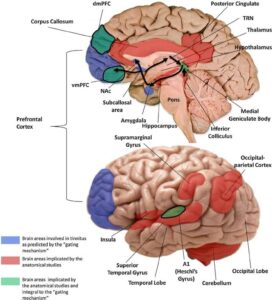
Neuroanatomical abnormalities in chronic tinnitus in the human brain
https://www.researchgate.net/publication/262816281_Neuroanatomical_abnormalities_in_chronic_tinnitus_in_the_human_brain – se nedladdad PDF
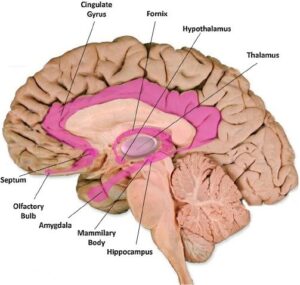
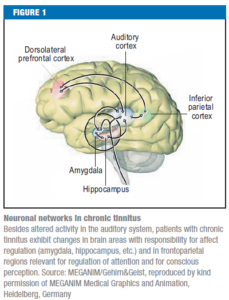
Fig. 1. Pathways and structures involved in tinnitus. Schematic of the ascending auditory pathways showing structures involved in tinnitus, from the cochlea to the auditory cortex in the brain. Human, but mainly animal studies of tinnitus have revealed increase in spontaneous activity, burst firing, and synchronous discharges at various stages of this pathway following lesions of the hair cells in the cochlea. These areas with structural and functional change in tinnitus are shown in blue, according to the review by Eggermont (2013).
Fig. 2. Limbic system structures. The various structures of the limbic system, shownin pink, some of which have been implicated in neuroimaging studies of tinnitus inhumans are involved in the processing of emotions.
Fig. 3. Neuroanatomical changes in tinnitus. Brain areas proposed to be involved in the gating mechanism (blue) and those discovered by anatomical MRI studies of tinnitus. Areas common to both are shown in green. Note that vmPFC and dmPFC were reported as effects of hearing loss rather than tinnitus (Melcher et al., 2013). The corona radiata and the longitudinal fasciculus are not shown. The arrows represent the flow of neural activity arriving at the IC and MGN and relayed to the primary auditory cortex for perception. The signal is then sent via the amygdala to the subcallosal region and the NAc for evaluation of emotional content. From here, the reticular nucleus of the thalamus receives an excitatory feedback, which inhibits the section of the MGN corresponding to the tinnitus sound (see Rauschecker et al., 2010).
Tinnitus, cervical spine instability, and neck pain
https://www.caringmedical.com/prolotherapy-news/tinnitus/
Video
https://youtu.be/jY0wsrohKwQ
https://youtu.be/yJ2QiJpD-UQ
”Vagus nerve compression has been implicated in many problems. In our clinical and research observations, we have documented that Prolotherapy can offer answers for sufferers of cervical instability, as it treats the problem at its source. Prolotherapy to the various structures of the neck eliminates the instability and the sympathetic symptoms such as tinnitus and related disorders without many of the short-term and long-term risks of cervical fusion. We concluded that in many cases of chronic neck pain, the cause may be underlying joint instability and capsular ligament laxity. Furthermore, we contend that the use of comprehensive Prolotherapy appears to be an effective treatment for chronic neck pain and cervical instability, especially when due to ligament laxity. The technique is safe and relatively non-invasive as well as efficacious in relieving chronic neck pain and its associated symptoms.
What are we seeing in this image?
A Digital Motion X-Ray or DMX is a tool we use to help understand a patient’s neck instability and how we may be able to help the patients with our treatments. In the illustration below a patient who suffered from upper cervical instability demonstrated hypermobility of the C1-C2. This hypermobility can result in common symptoms of neck pain, headaches, dizziness, vertigo, tinnitus, concentration difficulties, anxiety, TMJ, and other symptoms.”

The curvatures of the neck -What are we seeing in this image?
In our practice, we see problems of cervical spine instability caused by damaged or weakened cervical spine ligaments. With ligament weakness or laxity, the cervical vertebrae move out of place and progress into problems of chronic pain and neurological symptoms by distorting the natural curve of the spine. This illustration demonstrates the progression from Lordotic to Military to Kyphotic to “S” shape curve.
In this video, a demonstration of treatment is given
Prolotherapy is referred to as a regenerative injection technique (RIT) because it is based on the premise that the regenerative healing process can rebuild and repair damaged soft tissue structures. It is a simple injection treatment that addresses very complex issues.
This video jumps to 1:05 where the actual treatment begins.
This patient is having C1-C2 areas treated. Ross Hauser, MD, is giving the injections.https://youtu.be/QsP3DzbUacw
Tinnitus
https://www.physio-pedia.com/Tinnitus
“Clinically Relevant Anatomy – A neural connection between the somatosensory and the auditory systems may be important in tinnitus. Anatomical and physiological evidence support this statement. The trigeminal and dorsal root ganglia transfer afferent somatosensory information from the periphery to secondary sensory neurons in the brainstem. These structures send excitatory projections to the cochlear nucleus. Moreover, the cochlear nucleus innervates parts of the trigeminal, ophthalmic and mandibular nuclei. Signals from the trigeminal supply the hearing system in the cochlear nucleus, superior olivary nucleus, and inferior colliculus.[4]
Patients with chronic tinnitus exhibit changes in brain areas with responsibility for affect regulation (amygdala, hippocampus, etc.) and in frontoparietal regions relevant for regulation of attention and for conscious perception.[1]”
BvS-> Below more from this link highly interesting
Tinnitus, Cervical instability, and neck pain – https://www.caringmedical.com/prolotherapy-news/tinnitus/#:~:text=In%20mant%20of%20these%20patients,of%20cervical%20spine%2Fneck%20 instability.&text=%20eustachian%20tube%20is%20the,ear%20and%20the%20upper%20throat.
”People with tinnitus can benefit from many treatments. In this article, we will propose an aspect of tinnitus treatment, the relationship between tinnitus symptoms and cervical neck instability and treatments that strengthen the ligaments of the cervix. Repair of cervical necklaces in the cervix can lead to relief of tinnitus symptoms. Tinnitus can be a very complex condition to treat. Not all cases of tinnitus are caused by cervical carotid lesions. However, in this article we will discuss when neck ligament damage is suspected as the cause of hearing problems and as a possible reason why you have not responded to other treatments.
.. In many of these patients, their problems with tinnitus, Menieres disease, dizziness, ear fullness, decreased hearing or sensitivity to sound can be traced to problems with spinal/neck instability. The Eustachian tube is the canal that connects the inner ear and upper neck”
Secondary tinnitus as a symptom of instability of the upper cervical spine: crucial management
”Abstract: Tinnitus is very often caused by instability in the craniocervical junction. It very often manifests itself as a high-altitude whistle that disappears after operative correction and stabilization of articular geometry. Prolapsed intervertebral disks, discoligamentous lesion, and even metastases as low as level C3 can cause tinnitus, which also usually disappears after surgery. Keywords: alar ligament; instability. upper cervix” See PDF printing https://pubmed.ncbi.nlm.nih.gov/14689631/
Barre-Lieou Syndrome – https://piedmontpmr.com/diagnose-treat-barre-lieou-neck-pain-blurred-vision-nausea-vertigo-tinnitus-2/
”How can a disease cause all these problems?
The answer lies in the sympathetic nervous system (part of the autonomic nervous system) that monitors and regulates various activities that occur independently of the rest of the nervous system. Examples are student accommodation for light, balance in the inner ear and breathing.
If a structure intercalated by (or monitored by) the sympathetic system is damaged, it is the task of the sympathetic system to react to that damage. In the case of Barre-Leiou, posterior Cervical Sympathetic Chain forgets to stop monitoring the site of the damage; Like a car engine like diesel, it forgets to turn it off.
When this happens, the whole system becomes too sensitive to further stimulus. Shifting barometric pressure, stress or sinus infections can worsen symptoms. Treatment should be focused on restoring normal sympathetic nerve function, improving blood flow and reducing the overall load (the total number of things that do not allow the system to heal).
Diagnosis can be difficult, especially if the attending physician is not familiar with the disease. Thermography is a specialized study that measures skin temperature. It is an ideal test to evaluate for the presence of Barre-Lieou. More traditional studies include MRI (to exclude structural problems in the head and neck) and electrodiagnostic studies (to control nerve damage).
Medications, physiotherapy and sympathetic blocks (nerve blocks directed at the sympathetic system) are all used to restore physiology to normal and relieve symptoms. People with persistent head and neck pain, e.g. after a road accident, or with persistent migraines associated with blurred vision, numbness or tinnitus, should consider Barre-Lieou when seeking help.5