(Part of the blow ”2021 links on cervical instability” is translated into Swedish at http://carism.se/notes/klinisk-info-2021/cervikal-instabilitet-refluxer-och/ + some more info at http://carism.se/project/projekt-carism/hyperacusis/)
First a warning; The below is NOT readabl yet! PLease, do not read the below if you can not stand very incomplete and very unstructured texts – I let access to this link only for those who can deal with the below and believe they could get some idea from links, pictures,…
Why this warning? See below … but be careful …
Ongoing work while working during “severe inner alarms” (Tinnitus, 24/Day conditions since October 2019) as well as I can only work 15-20 minutes until increased ”alarm” prevent further work for hours! This explains that the below is very raw, incomplete text and structures but, in spite of this, I leave access this overview with many links, if anybody could have use of it! I will work hard as well I can also with language/layout/structured in a more logical way etc. … …
(last updated 2020-09-09 – much info is waiting to be inserted here – when possible)
Content list after the introduction below
Introduction (Prelude is moved from here to an under tab to this one)
Below mainly texts from some (as I see it) important links on aspects/findings/arguments.. on what is needed to work from a multidisciplinary integrated paradigm within complex multifaceted kinds of Tinnitus. NB it is mainly to give an overview of what is going on – that is, highlight multifaceted (clinical real worlds) approaches/perspective …
I will elsewhere elaborate much more the below!
Below is an overview of what I have found within the (for me very new) field of multifaceted Tinnitus syndromes, really a multidisciplinary evolution exploding – quite different from e.g. exploding head syndromes suffering without any clinical support – which needs to be multidisciplinary systems integrated enabled to individually identified with biopsychosocial effective examinations, diagnosis working hypotheses following up effective adjusted interventions, where patients can be regarded via practical education a resource and not just a problem!
As you will see, below, it is quite a lot of more or less fragmentary knowledge/argument/opinion/hypotheses … giving a straggly impression, very much needed are systems integrating multifaceted, multidisciplinary model building, simulator bench testing and pre-clinical evaluation work before introduction into clinical settings. For us suffering a long time to go still … so who take the lead, politicians, those in medical power positions, … patients?
Meanwhile I have been working with this link (5 month), I am happy to see that more and more happens within this field, at least internationally – Hope more happens in Sweden then what I know of!
This include also more non-reducionistic approaches with systems integrating explanations and practical measures! And, it seems that this is increasing!
Content:
Patient Navigator – American Tinnitus Association – with a comprehensive picture
Comprehensive contributes more or less multidisciplinary
Cervical Tinnitus
Tinnitus treatment when there are symptoms of cervical spine instability
Secondary Tinnitus as a Symptom of Instability of the Upper Cervical Spine: Operative Management
2021 links on cervical instability
Cervicocranial Tinnitus syndrome
Hydrocephalus and Cerebrospinal Fluid (CSF) Leaks
Trigeminal neuralgia: Pathology and pathogenesis
Auditory nerve compression: a forgotten treatable cause for tinnitus
Hyperactivity in the auditory brain follows cochlear damage?
Middle Ear Myoclonus
Otoacoustic Emissions
The inner ear and the neurologist
Cochlea Migraine (without headache)
Tinnitus and Headache
Cochlea and Tinnitus
Two main pathways from cochlea
GABA and Glutamate – neurotransmittor imbalance
Hair cells – outer and inner functions
Mitochondria and Tinnitus
The role of mitochondrial oxidative stress in hearing loss
Microcirculation and Tinnitus
Herpes zoster and Tinnitus
Refluxes and Tinnitus
Inflammaging and Hearing dysfunctions
How is endoymfatic hydrops produced, what influence it and what can we do clinically?
Endolymfatic Hydrops and Eustachian dysfunctions
Endolymph Drainage System in Meniere’s Disease
About Eustachian Tube Dysfunction
Eustachian Tube Dysfunction and Tinnitus
Eustachian tube dysfunctions and Sinus problems
Secondary Endolymfatic Hydrops (SEH)
Weather, Tinnitus and especially Endolymfatic Hydrops
SEH clinical approaches
How is airwax produced?
Orienting Response, Habituation, Locus Coeruleus and RAS
Reticular activation System, RAS
Habituation and different severe kinds of Tinnitus
Autonomic nervous system and Tinnitus
How to influence severe Tinnitus with Vagus
Psychological interventions and Tinnitus
Sense Of Coherence (SOC) and Tinnitus
Multidisciplinary Systems Integration
…..
Towards an objectification by classification of tinnitus
Tests/examinations/…
Intervention overview
Meniere’s Disease Diet
Swedish activities/examinations/interventions/presence of different types of Tinnitus in the population
My case
My message to Tinnitus colleagues
Main recerences
Patient Navigator – American Tinnitus Association
Inserted 2020-09-07
https://www.ata.org/managing-your-tinnitus/tinnitus-patient-navigator
See especially; OTOLARYNGOLOGIST
“(a.k.a. ENT): A medical doctor who specializes in the evaluation and treatment of disorders of the ears, nose and throat and related structures of the head and neck. An otolaryngologist can rule out physical causes of tinnitus such as excessive ear wax, problems with the middle ear (e.g., fluid, stiffened bones), or benign tumors on the auditory nerve. Otolaryngologists work in private practices, academic medical centers, community health centers and hospitals.” … as well as “NEUROTOLOGIST: A medical doctor who has trained in the field of otolaryngology-head and neck surgery and evaluates and manages neurological disorders of the ear. See Otolaryngologist”. https://www.ata.org/managing-your-tinnitus/tinnitus-patient-navigator
Also -> https://med.uth.edu/orl/online-ear-disease-photo-book/chapter-4-fluid-in-the-ear/fluid-in-the-ear-discussion/ main link https://med.uth.edu/orl/
Comprehensive contributes more or less multidisciplinary
Here I will put together comprehensive contributes I find – continuously updated;
Pathophysiology, Diagnosis and Treatment of Somatosensory Tinnitus: A Scoping Review – https://www.frontiersin.org/articles/10.3389/fnins.2017.00207/full – “Discussion and Conclusions: Despite the apparent prevalence of somatosensory tinnitus its underlying neural processes are still not well understood. Necessary involvement of multidisciplinary teams in its diagnosis and treatment has led to a large heterogeneity of approaches whereby tinnitus improvement is often only a secondary effect. Hence there are no evidence-based clinical guidelines, and patient care is empirical rather than research-evidence-based. Somatic testing should receive further attention considering the breath of evidence on the ability of patients to modulate their tinnitus through manouvers. Specific questions for further research and review are indicated”.
Cervical Tinnitus
Predicting the Risk of Hearing Impairment Following the Cervical Spine Diseases by Measuring the Cervical Range of Movements: A Pilot Study – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5691173/
“Cervical spine abnormalities can affect the ear vessels and or nerves with different mechanisms. Ear dysfunctions following cervical spine injuries can be manifested as hearing loss, vertigo, or tinnitus.” … “The hearing impairment following the cervical spine diseases (such as osteoarthritis, rheumatoid arthritis, disk herniation at cervical upper segments, whiplash, etc.) may appear as hearing loss, vertigo, and tinnitus “
Cervical Spine Disorders and its Association with Tinnitus: The ”Triple” Hypothesis https://chiro.org/Subluxation/Cervical_Spine_Disorders.shtml
“Subjective tinnitus and cervical spine disorders (CSD) are among the most common complaints encountered by physicians. Although the relationship between tinnitus and CSD has attracted great interest during the past several years, the pathogenesis of tinnitus induced by CSD remains unclear.
Conceivably, cervical spine disorders could trigger a somatosensory pathway-induced disinhibition of dorsal cochlear nucleus (DCN) activity in the auditory pathway; furthermore, CSD can cause inner ear blood impairment induced by vertebral arteries hemodynamic alterations and trigeminal irritation.
In genetically -predisposed CSD patients with reduced serotoninergic tone, signals from chronically stimulated DCNs could activate specific cortical neuronal networks and plastic neural changes resulting in tinnitus. Therefore, an early specific tailored CSD treatments and/or boosting serotoninergic activity may be required to prevent the creation of ’tinnitus memory circuits’ in CSD patients”.
Predicting the Risk of Hearing Impairment Following the Cervical Spine Diseases by Measuring the Ce rvical Range of Movements: A Pilot Study
Conclusion: According to the present study, the likelihood of hearing loss was high in patients with cervical left rotation limitation, and that the incidence of hearing loss following the cervical spine injuries was more in men. It seems that left Rotation limitation can be used as a predictor to diagnosis of hearing impairment following the cervical spine injuries (especially in men). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5691173/
Cervical Tinnitus https://www.dizziness-and-balance.com/disorders/hearing/tinnitus/cervical%20tinnitus.html
“A rare source of tinnitus is damage to the neck. The concept here is not that the neck injury creates sound, but rather that neck input can modulate brainstem structures that are involved in sound generation. We believe it to exist based on cases that we have encountered through the years in our clinical practice. We think that cervical tinnitus is rare. However, there are some authors that state that it occurs ”very often” (Montazem, 2000). A systemic review in 2018 that included 24 papers on the subject stated that ”There is weak evidence for an association between subjective tinnitus and CSD.” (Bousema et al, 2018).”
Anterior Cervical Osteophytes and Sympathetic Hyperactivity in Patients with Tinnitus: Size Matters
https://www.researchgate.net/publication/330479680_Anterior_Cervical_Osteophytes_and_Sympathetic_Hyperactivity_in_Patients_with_Tinnitus_Size_Matters
Context: Pathological changes secondary to degeneration of the cervical intervertebral disc may cause irritation of sympathetic nerve fibers, leading to sympathetic symptoms and tinnitus. Objectives: The aim of this study was to relate the effect of percutaneous radiofrequency treatment of superior cervical sympathetic ganglion in patients with tinnitus to cervical pathology. Method: A retrospective study of 74 consecutive patients who underwent treatment of the superior cervical sympathetic ganglion for tinnitus that persisted for 1 month or longer from October 2016 to January 2018. The work-up of a patient with tinnitus consisted of a standardized clinical history, a bilateral audiogram and a cervical spine radiograph. Results: All patients had a test blockade of superior cervical sympathetic ganglion first, and 54% of these patients (n=40) responded with a reduction of their tinnitus. These patients underwent a radiofrequency lesion and 53% (n=21) responded with a reduction of their tinnitus at 7 weeks following treatment. The size of anterior osteophyte at the fifth cervical vertebrae was related to a positive response at 7 weeks following this treatment. Patients with tinnitus and an anterior osteophyte at vertebrae C5 more than 17% of the width of those vertebrae had a success rate of 52% following treatment of the superior cervical sympathetic ganglion, compared to 13%, when the anterior osteophyte at C5 was 17% or less. Conclusions: The size of anterior cervical osteophytes is associated with a higher success rate of radiofrequency lesions of the superior sympathetic ganglion for tinnitus. The current results imply a role for cervical sympathetic nervous system irritation in the development of tinnitus in a subgroup of patients.
Assessment of temporomandibular and cervical spine disorders in tinnitus patients
https://www.sciencedirect.com/science/article/pii/S0079612307660191
In treating patients with temporomandibular joint (TMJ) dysfunction it was noticed that tinnitus and vertigo were common in such patients and there was also muscular tension in jaw and neck. During treatment of these patients it was also noted that injection of lidocaine in a jaw muscle (m. pt. lat.) reduced not only their muscular problems but also that the tinnitus was reduced while the local anesthetic was active. Evaluation of 39 patients with disabling tinnitus, and all suffered from tinnitus, revealed that 10 of them had bilateral tinnitus and TMJ disorders revealed that pain in the face, temples or jaw occurred often among these patients. Many of such patients had also symptoms of cervical spine disorders, head, neck and shoulder pain, and limitations in side bending and rotation were also frequent complaints. One-third of these patients could influence tinnitus by jaw movements and 75% could trigger vertigo by head or neck movements.
Treatment of jaw and neck disorders in 24 patients with Ménière’s disease had a beneficial effect on not only their episodic vertigo but also on their tinnitus and aural fullness. At the 3-year follow-up, intensity of all symptoms were significantly reduced (p<0.001).
Cervical Spine Dysfunctions in Patients With Chronic Subjective Tinnitus
To assess, characterize, and quantify cervical spine dysfunction in patients with cervicogenic somatic tinnitus (CST) compared to patients suffering from other forms of chronic subjective non-pulsatile tinnitus. Cross-sectional study. Tertiary referral center. Consecutive adult patients suffering from chronic subjective non-pulsatile tinnitus were included. Exclusion criteria: Ménière’s disease, middle ear pathology, intracranial pathology, cervical spine surgery, whiplash trauma, temporomandibular dysfunction. Assessment comprises medical history, ENT examination with micro-otoscopy, audiometry, tinnitus assessment, temporomandibular and cervical spine investigation, and brain MRI. Patients were classified into CST and non-CST population. Cervical spine dysfunction was investigated using the Neck Bournemouth Questionnaire (NBQ) and clinical tests of the cervical spine, containing range of motion, pain provocation (adapted Spurling test, AST), and muscle tests (tenderness via trigger points, strength and endurance of deep neck flexors). Between-group analysis was performed. The prevalence of cervical spine dysfunction was described for the total group and for CST and non-CST groups. In total, 87 patients were included, of which 37 (43%) were diagnosed with CST. In comparison with the non-CST group, the CST group demonstrated a significantly higher prevalence of cervical spine dysfunction. In the CST group, 68% had a positive manual rotation test, 47% a positive AST, 49% a positive score on both, and 81% had positive trigger points. In the non-CST group, these percentages were 36, 18, 10, and 50%, respectively. Furthermore, 79% of the CST group had a positive NBQ versus 40% in the non-CST group. Significant differences between the both groups were found for all the aforementioned variables (all p <0.005). Although a higher prevalence of neck dysfunction was found in the CST group, neck dysfunction is often in non-CST patients.
Cervical Trigger Point Acupuncture for Treatment of Somatic Tinnitus
https://www.sciencedirect.com/science/article/pii/S2005290119300032
Cervicogenic somatic tinnitus is a subtype of subjective tinnitus and is defined as tinnitus in which forceful contractions of jaw and neck muscles modulate its psychoacoustic attributes. Various physical therapies have been proposed for the treatment of somatosensory tinnitus although there is no definitive cure for it. This report describes the use of acupuncture in the treatment of a 71-year-old woman with chronic neck pain who suffered from a left-sided tinnitus for 2 years as well. The tinnitus and neck pain severity was rated as 7 and 6, respectively, on a numeric rating scale of 10. On examination, she had restricted cervical range of motion and several myofascial trigger points in cervical muscles. Audiometric tests of the patient were normal. She received trigger point acupuncture of cervical muscles twice per week for 10 sessions. Her tinnitus completely disappeared after the third session and did not return during the 5-year follow-up. Her neck pain intensity also decreased to 1 on the numeric rating scale after 10 sessions. Based on the results of this study, direct trigger point acupuncture of cervical muscles may be beneficial in the treatment of somatic tinnitus with a long-duration effect.
Tinnitus Is Often Described As Ringing In The Ears, But Is A Complex Condition – https://www.necksolutions.com/tinnitus/ BvS-> A very comprehensive text!
“……” A thorough history and examination by a health care provider is vital, considering possible causes related to cardiovascular, thyroid, tumors and a variety of medications, which include many commonly used pain relievers. Frustratingly, many investigations fail to locate a cause. However, eliminating very concerning causes like tumors is important to relieve some of the stress.
There are many possible causes and this stresses that it is vital to have an evaluation by a health care professional. Factors involved may be loss of hearing, especially high frequency hearing loss, dizziness related to an inner ear disorder, blockage in the ear, hyperacusis – a sensitivity to noise, tumors, inflammation of the ear, sinus problems, headache and vascular disorders, metabolic disorders related to sugar like diabetes, thyroid or lipids, cervical arthritis, hormonal problems, stressful situations, anxiety, depression, medications that are toxic to the ear (ototoxic), stimulants, epilepsy and other disorders.”
… much interesting text/references about “tinnitus related to neck problems”, “Somatosensory Tinnitus”, “Brain function”,
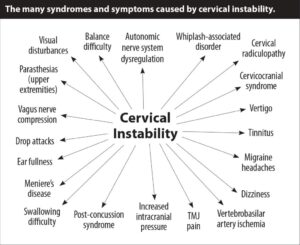
BvS-> No particular text to the above illustrative picture, but as it shows a common reasons for Tinnitus I put it in here in anyway
As well as “Are There Natural Supplements To Help?” About Magnesium, Malatonin, Ginko, Zinc (hypozincemia), B12, B2, B3, Water & Protein, coffee (had a protective effect on tinnitus, and the relationship was dose dependent; the higher frequency of coffee drinking had more of a protective effect. Brewed coffee had more of an effect than canned or instant in those 40 to 64 years age group. These results suggest a protective effect of coffee on hearing loss and tinnitus).
Furthermore -> “Can antibiotics help? Sound Therapy, EMDR, Intratympanic Steroid Therapy, and -> Do You Experience Tinnitus In Your Dreams? (a study indicated tinnitus is not experienced when dreaming. They investigated 78 patients at a specialized research clinic, of which 97% did not experience tinnitus in their dreams. They hypothesized that during dreaming, a prediction error from interacting with the environment in tinnitus is not present”).
Tinnitus treatment when there are symptoms of cervical spine instability
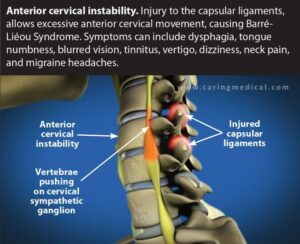
 https://www.caringmedical.com/prolotherapy-news/tinnitus/
https://www.caringmedical.com/prolotherapy-news/tinnitus/
“So there is a connection between temporomandibular disorders and tinnitus, but there seems to be a missing link”.
Something is missing in this puzzle. In our opinion at Caring Medical, it is a diagnosis of cervical instability.” “Tinnitus can be triggered by cervical neck instability, TMJ-TMD can be triggered by cervical neck instability. Tinnitus can be caused by temporomandibular disorders” .. “something is missing, in a tinnitus examination. It is a look at the neck”.
Tinnitus and the Relationship to Upper Neck Problems https://uppercervicalawareness.com/the-relationship-between-tinnitus-and-upper-cervical-problems/
Connection With the Upper Neck: The top bone in the neck, located right at the base of the skull, is called the atlas (C1 vertebra). This bone is positioned almost directly between the ears and jaw joints. As a result, everything in this part of the body can be affected by even the slightest misalignment. That’s why ear and jaw problems often go together, and why many who suffer from these issues may also have neckaches.
Misaligned Atlas and the Ringing Ears: For one thing, a misaligned atlas can affect the structures of the ear. The eustachian tubes, in particular, play a vital role. These tubes drain away excess fluid from the ears so they can drain harmlessly. However, if tube function is inhibited, fluid can build up and lead to tinnitus. Therefore, even when ringing in the ears is caused by a blockage, the problem may still be in the neck.
Diagnosis and management of somatosensory tinnitus: review article – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3129953/
” Tinnitus is the perception of sound in the absence of an acoustic external stimulus. It affects 10–17% of the world’s population and it a complex symptom with multiple causes, which is influenced by pathways other than the auditory one. Recently, it has been observed that tinnitus may be provoked or modulated by stimulation arising from the somatosensorial system, as well as from the somatomotor and visual–motor systems. This specific subgroup – somatosensory tinnitus – is present in 65% of cases, even though it tends to be underdiagnosed. As a consequence, it is necessary to establish evaluation protocols and specific treatments focusing on both the auditory pathway and the musculoskeletal system.”
BvS …. Much detailed informative text …
“conclusion; Studies have been pointing towards a high prevalence of somatosensory tinnitus among tinnitus patients. Thus, professionals involved with providing treatment for patients with tinnitus must differentiate this specific subgroup from the conventional ones. Investigating the presence of somatosensory tinnitus by means of a specific protocol and choosing adequate therapeutic options that will target auditory pathways and musculoskeletal disorders may increase the possibility of satisfactory results”.
Chronic Cervicogenic Tinnitus Rapidly Resolved by Intermittent Use of Cervical Collar – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4803736/ “In a single case of chronic tinnitus, we found that treatment with CC rapidly led to full remission. Blood flow reduction in vertebral arteries was unrelated to tinnitus. However, tinnitus could be resumed by constrained head postures. Experimental tinnitus replication (by inclination) points to an underscored role of upper posterior cervical muscle groups, matching with animal experiments, also in concert with other triggers including psychological factors”.

See also https://www.physio-pedia.com/Cervical_Collar
I will begin 2020-09-18 to evaluate the Vista Collar below
https://embreis.com/se/vistahalskrage
The Role of Physical Therapy in Tinnitus Management – https://www.ncrar.research.va.gov/Conference/Documents/PPT/CherianK.PDF
Secondary Tinnitus as a Symptom of Instability of the Upper Cervical Spine: Operative Management
Tinnitus very often is caused by instability of the craniocervical junction. It very frequently manifests as a high-pitched whistle that disappears after operative correction and stabilization of the articular geometry. Prolapsed intervertebral disks, discoligamentous injury, and even metastases as low as level C3 can cause tinnitus, which also usually disappears after surgery. https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwih8s-Nn53rAhVsxosKHU7HAYIQFjAEegQIBBAB&url=http%3A%2F%2Fwww.tinnitusjournal.com%2Farticles%2Fsecondary-tinnitus-as-a-symptom-ofinstability-of-the-upper-cervical-spineoperative-management.pdf&usg=AOvVaw3Z2AvIeqbzq3nGm21Ke5fw
2021 links on cervical instability
Below much from the link below – but there are much more valuable info at the link!
Cervical Instability: Causes, Symptoms, & Treatments
https://denveruppercervical.com/cervical-instability/
- Feeling that your skull may “fall off” the spine
- Occipital headaches
- Migraines
- Muscle spasms
- Neck, shoulder, or jaw pain
- Difficulty swallowing
- Tenderness at the base of thee skull
- Light sensitivity
- Blurred vision
- Tinnitus (ringing in the ears)
- Orthostatic intolerance
- Tremors
- Vertigo
- Dizziness
- Clumsiness
- Fainting
- Limb weakness
- Shortness of breath
- Nausea
- Fatigue
- Lhermitte’s sign
- Cognitive decline
- Memory loss
Diagnosing Cervical Instability
How do you test cervical instability? Here are 4 testing methods for cervical instability:
- Upright MRI (AKA magnetic resonance imaging)
- Supine MRI (laying on your back)
- CT scan (AKA computerized tomography)
- Digital x-ray
It is worth mentioning that, although MRIs are the most common diagnostic testing method for cervical instability, a 2012 scientific investigation found that MRIs had “limited diagnostic value in patients with whiplash-associated disorders” such as cervical instability.
Here are some measurements doctors will look for to diagnose cervical instability:
- Clivo-Axial Angle less than or equal to 135 degrees
- Grabb-Oakes measurement greater than or equal to 9 mm
- Harris measurement greater than 12mm
- Any spinal subluxation
Causes of Cervical Instability
Craniocervical instability is caused by ligament laxity between the skull and the top two vertebrae (the atlas and the axis). This allows excessive movement and leads to a long list of physical and neurological symptoms.
These factors can cause ligament laxity and result in cervical instability:
- Whiplash or other injury
- Connective tissue disorders, such as Ehlers-Danlos Syndrome or rheumatoid arthritis
- Tethered cord syndrome
- Chiari malformation
- Genetics
https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=bdee757bc826f7b8bd497a22b63357cf61eec8bd
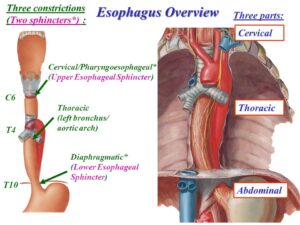
(BvS) Hypotheses Diagnoses Reasoning: The above “Vertebrae pushing …” motivate including local sympathetic nervous systems (SNS) dysfunctional activity and as Refluxes (mostly silent but sometimes very typical symptoms) also can behave dysfunctional due to not functional SNS and since refluxes during many years are part of my own “symptoms picture” cervikal instability can interplay/influence Pharyngoesophageal (esophageal) sphincter functioning – as the sphincter function “reversed” = increased SNS increase it decrease esophageal sphincter muscles functioning = facilitate reflux behaviros – much info at https://www.ncbi.nlm.nih.gov/books/NBK557452/ see also below picture
https://slideplayer.com/slide/7891920/
More reasoning based on my own experiences from actual patient position; “While people can experience GERD (gastro-esophageal reflux disease) and back pain at the same time, it is more likely that the GERD is caused by something related to the existing back pain or its treatment, rather than GERD causing back pain. Here are some possible causes of GERD and acid reflux related to back pain—and how to handle them” https://www.spine-health.com/blog/can-gerd-cause-back-pain
But also silent refluxes and refluxes via “Reciprocal Causal Relationship between Laryngopharyngeal Reflux and Eustachian Tube Obstruction” http://medcraveonline.com/JOENTR/JOENTR-02-00046.pdf is not to be forgotten.
One symptom change (increase) observation may give diagnoses hypotheses reasoning material? It is during the nights (last 20 years I sleep 8-10 h excellent) but since this hard permanent blasting symptoms emerged (October 2019) a pronounced increase always developed last 2-3 hours together (in parallel) with increased back (lumbal?) pain (have MRI data on L4-L5 foraminala stenoses and S1 disc herniation) and a two point neck (moderate) pain. Interplay between ???
Also strange that reflux symptoms develop during exercise cycling but not during treadmill exercise.
Moreover; About refluxes and tinnitus – https://www.betterbalanceinlife.com/the-gut-and-vertigo/ “If you have acid reflux (or heartburn) and dizziness, I think this article may be interesting to you…… I think the author presents a very interesting idea that the “refluxed material” can be aggravating the Eustachian tubes which run from the middle ear to the back of the throat.
I’ve had patients with vertigo episodes related to acid reflux.
This association is called “acidic labyrinthitis” and can result in tinnitus, dizziness, and vertigo.
The refluxed food particles and the stomach acids can irritate the ear, though the eustachian tube which connects the throat to the ear.
Esophagitis, or inflammation of the esophagus, is often involved due to the throat irritation as well”. .. Then suddenly in December, got acid reflux. I’d never had that before in my life, also never woke up with throat sensations/sinus/nose etc which might have made me suspect a silent reflux ..
… I .. went to a GI doctor, who basically just looked at me as if I was crazy and laughed at me for asking if I was dizzy because of acid reflux!!! Dr Bell answers the above: You may have silent reflux and/ or esophagitis ….”
Taken together; Cervikal instability and silent refluxes can cause a number of symptoms where I focus on what are most symptoms driven in hypotheses diagnostic reasoning. As clinical examinations are complex and not always clearly can identify without different assessment approaches, I use psychophysiological tools from the toolbox which – given above reasoning is wrong – do not harm but in stead are part of my health promotion activities I enjoy!
Synopsis; Knowledge development concerning the gut-brain axis motivate really open mind for systems interactions, especially we probably will more in general increase our undertanding of omplex biopsychosocial medicine interplay (www.biopsychosocialmedicine.com)
Tinnitus, cervical spine instability, and neck pain – https://www.caringmedical.com/prolotherapy-news/tinnitus/#:~:text=In%20many%20of%20these%20patients,of%20cervical%20spine%2Fneck%20instability.&text=The%20eustachian%20tube%20is%20the,ear%20and%20the%20upper%20throat.
“People with tinnitus can find benefit in many treatments. In this article, we will suggest one aspect of tinnitus treatment, the connection of tinnitus symptoms to cervical neck instability and treatments that strengthen the cervical spine neck ligaments. Repairing cervical spine neck ligaments can lead to an alleviation of tinnitus symptoms. Tinnitus can be a very complex condition to treat. Not all cases of tinnitus are caused by cervical neck ligament damage. In this article, however, we will discuss when cervical neck ligament damage is suspected as the cause of hearing issues and as a possible reason why you have been unresponsive to other treatments.
.. In many of these patients, their problems of tinnitus, Meniere’s disease, dizziness, ear fullness, decreased hearing, or sensitivity to sound may be traced to problems of cervical spine/neck instability. The eustachian tube is the canal that connects the inner ear and the upper throat”
Secondary tinnitus as a symptom of instability of the upper cervical spine: operative management
“Abstract: Tinnitus very often is caused by instability of the craniocervical junction. It very frequently manifests as a high-pitched whistle that disappears after operative correction and stabilization of the articular geometry. Prolapsed intervertebral disks, discoligamentous injury, and even metastases as low as level C3 can cause tinnitus, which also usually disappears after surgery. Key Words: alar ligament; instability; upper cervical spine” See PDF printout https://pubmed.ncbi.nlm.nih.gov/14689631/
Barre-Lieou Syndrome – https://piedmontpmr.com/diagnose-treat-barre-lieou-neck-pain-blurred-vision-nausea-vertigo-tinnitus-2/
“How can one disorder cause all of these problems? The answer lies within the sympathetic nervous system (a portion of the autonomic nervous system) that monitors and regulates various activities that occur independently from the rest of the nervous system. Examples include pupil accommodation to light, equilibrium within the inner ear, and respiration.
If a structure that is innervated by (or being monitored by) the sympathetic system becomes injured, then it is the job of the sympathetic system to react to that injury. In the case of Barre-Leiou, the Posterior Cervical Sympathetic Chain forgets to stop monitoring the injury site; like a car engine that diesels, it forgets to shut down.
When this happens, the entire system becomes overly sensitive to any further stimulus. Shifting barometric pressure, stress, or sinus infections can make symptoms worse. Treatment should be directed toward restoring normal sympathetic nerve function, enhancing blood flow, and reducing total load (the total number of things that do not allow the system to heal).
Diagnosis can be difficult, especially if the treating physician is not familiar with the disorder. Thermography is a specialized study that measures skin temperature. It is an ideal test to evaluate for the presence of Barre-Lieou. More traditional studies include MRI (to rule out structural problems in the head and neck) and electrodiagnostic studies (to check for nerve damage).
Medications, physical therapy and sympathetic blocks (nerve blocks directed toward the sympathetic system) are all used to restore physiology to normal and relieve symptoms. People with persistent head and neck pain, such as after a motor vehicle accident, or with persistent migraine associated with blurred vision, numbness or tinnitus, should consider Barre-Lieou when looking for help.
Cervicocranial Tinnitus syndrome
Cervicocranial Syndrome https://www.sbshospital.com/cervicocranial-syndrome/
Cervicocranial syndrome is also known as Barre-Lieous syndrome and refers to a complex combination of neurological symptoms. These symptoms usually include chronic headache, tinnitus (ringing in the ears), neck pain, facial pain, sinus pain, ear pain and pain at the carotid artery region. Other symptoms include dysphagia or difficulty in swallowing, allergies, dizziness and vertigo. Some patients also complain about a chronic, dull throbbing pain at the base of the skull, which worsens upon movement of the head or neck.
This group of symptoms is believed to be caused by a misalignment of the cranial bones and the cervical bones of the spine. The syndrome can present independent of age, disease or associated trauma in a person. It is believed that the syndrome could also arise due to damage to the posterior cervical sympathetic chain consequent to the degeneration of the cervical vertebra leading to a prolapsed disc in the mid-cervical spine region.
The abnormalities in the skeletal structure in this syndrome result in exertion of undue pressure on the surrounding nerves. This pressure could be due to a gradual build-up of pinched nerves or it could be of sudden onset due to some trauma or injury. It could also be due to congenital abnormalities, arthritis, whiplash injury, rheumatoid arthritis or detrimental postural changes.
An ideal test for diagnosing cervicocranial syndrome is by the use of thermography to detect inflammation for uncovering medical issues. This test employs the use of an infrared camera to detect heat patterns and blood flow. Hypothermic areas were found over the cervical region and along the upper extremities in patients clinically diagnosed with cervicocranial syndrome. Basically a thermographic device displays heat emissions from the body as colored images of varying intensities and Chiropractors believe they can use it to detect areas of nerve pinching or impingement. A more traditional MRI imaging can also be done to rule out other problems of the neck which could be causing this syndrome.
Treatment usually entails the use of sympathetic nerve blocks or physical therapy. Subtle manipulation of the head and the cervical spine can help in realigning the bones back into their correct position and reducing head and neck pain. Other recommended therapies include neck stretches, postural training and trigger point therapy. While pain medications can help provide relief to some patients, others might need surgery to correct the subluxation of the cervical spine and decompression of spinal nerves.
If you are looking for help for similar symptoms, then you should avail the expertise of the formidable team of highly-qualified spinal specialists in the Sita Bhateja Specialty Hospital in Bangalore. These doctors are renowned for their medical skills in treating delicate conditions related to the spine and are backed by the most up-to-date technologies available. Check here for further details:https://www.sbshospital.com/”
Cervicocranial syndrome https://www.ncbi.nlm.nih.gov/medgen/386638 and https://en.wikipedia.org/wiki/Cervicocranial_syndrome
See also https://www.tspain.com/blog/what-is-cervicocranial-syndrome
BvS-> Although Cervicocranial syndrome contents much more than Tinnitus, I think that the avpbe and below can possibly be covered during this concept.
https://www.tinnitus.org.uk/somatic-somatosensory-tinnitus
Somatic/ Somatosensory Tinnitus
https://www.tinnitus.org.uk/somatic-somatosensory-tinnitus
… “The somatosensory system is a part of the sensory nervous system. This is a complex network of sensory and neurons that respond to changes at the surface or inside the body. These changes can include movement, pressure, touch, temperature or pain. Somatic (also called somatosensory) tinnitus (ST) is a subtype of subjective tinnitus, where changed somatosensory information from the cervical spine or jaw area causes or changes a patient’s tinnitus perception. Since Levine’s first publication in 1999 (1), several animal and human studies have found connections between the somatosensory system of the cervical (neck) and temporomandibular (jaw joint) area and the cochlear nuclei (CN), offering a physiological explanation for ST (2-4).
According to these studies, cervical or temporomandibular somatosensory information is transported to the brain by neural fibres from cell bodies located in the dorsal root ganglia or the trigeminal ganglion. Some of these fibres also project to the central auditory system. This enables the somatosensory system to influence the auditory system by altering spontaneous rates or synchrony of firing among neurons in the CN, inferior colliculus or auditory cortex. In this way, the somatosensory system is able to alter the pitch or loudness of the tinnitus (5).”
Hydrocephalus and Cerebrospinal Fluid (CSF) Leaks
Tinnitus as the first clinical manifestation of hydrocephalus
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1532-5415.1996.tb05656.x
” According to Meador,6 the physiopathogenic mechanism inducing tinnitus in the HTIC (Hypertensive intracraneal syndrome ) is a venous noise resulting from the turbulence created when the blood flows from the hypertensive intracraneal portion to the low‐pressure zone of the jugular bulb. This noise is unilateral owing to the assymmetry of the right and left jugular flow (anatomical variant of normality). Tinnitus is located on the side with the greater venous flow. This theory is supported by its direct relationship with intracraneal pressure (when the intracraneal pressure decreases, so does the tinnitus), its occurrence in front of the external auditory canal, its pulsating character, and its attenuation by maneuvers that decrease jugular flow (ipsilateral jugular compression, Valsalva maneuver and ipsilateral head movement). The finding of a pulsating tinnitus responding to jugular compression or to the Valsalva maneuver, may suggest HTIC. Both subjective and objective tinnitus have been associated with increased intracraneal pressure.4-6 Tinnitus has been seen in cases of idiopathic communicating hydrocephalus, pseudotumor cerebri, and primary brain tumor.6 In the case reported, the tinnitus was caused by increased intracraneal pressure attributable to hydrocephalus secondary to right laminal and cerebellar intraparenchymal hematomas.
The tinnitus disappeared spontaneously when the hydrocephalus remitted after treatment of the cerebral edema. The tinnitus caused by an idiopathic communicating hydrocephalus remits temporarily with repeated lumbar punctions and completely when peritoneal ventricular shunts or shunts from the lateral ventricle to the cisterna magna are made, whereas cases of tinnitus attributable to pseudotumor cerebri are also alleviated by repeated lumbar punctures.6-8 The interest of our case report is the presence of tinnitus as an advisory symptom of a HTIC syndrome. In conclusion, the presence of tinnitus in a patient with a recent history of cerebrovascular disease can point to the existence of an HTIC or hydrocephalus, this diagnosis being most likely when the tinnitus responds to jugular compression or to the Valsalva maneuver.”
Low pressure hydrocephalus https://en.wikipedia.org/wiki/Low_pressure_hydrocephalus
Patients with pulse-synchronous tinnitus should be suspected to have elevated cerebrospinal fluid pressure https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6753529/
“This study was performed to evaluate the prevalence and clinical importance of elevated cerebrospinal fluid (CSF) pressure among patients with pulse-synchronous tinnitus … Conclusions; If detailed physical and imaging examinations fail to detect the definite cause of pulse-synchronous tinnitus, a routine lumbar puncture should be performed to measure the CSF pressure. Elevated CSF pressure should be suspected in patients with pulse-synchronous tinnitus.”
Orthostatic headaches, tinnitus, and signs of connective tissue disorders may increase clinical suspicion of a spinal fluid leak
CSF (spinal fluid leak) leaks may cause tinnitus. “You can get ringing in the ears when you have migraine,” Dr. Carroll said. But if patients have tinnitus when they are not having headaches, “you should be thinking that there is something else going on.” Data suggest that CSF fluid is connected to inner ear fluid so a change of pressure in CSF changes inner ear pressure, and patients with high or low CSF pressure may get tinnitus.
Other symptoms may include neck pain and fatigue. “I have had the parents of patients tell me that the most remarkable thing that they see when we patch their sons or daughters is how they are bouncing around the house,” he said. Many patients complain of difficulty with concentrating, task persistence, and other nondescript, nonfocal neurologic symptoms.
Cerebrospinal Fluid (CSF) Leaks – https://www.dizziness-and-balance.com/disorders/central/csf-leak.html
“Of these symptoms, neck pain or stiffness, nausea and vomiting are the most common symptoms. If we consider which symptoms are the most specific, this is obviously #3. The associated symptoms are common human complaints — for example, severe tinnitus is endorsed by 6% of the population, and migraine headaches which commonly include photophobia and nausea affect roughly 15% of the entire population. Regarding #3, It has been our observation that brain MRI showing indirect signs of CSF pressure (i.e. dural enhancement) is rare.
Shievink et al (2016) observed that CSF leaks at the level of the skull base — e.g. CSF rhinorrhea, do not cause spontaneous intracranial hypotension, and presumably then, do not cause orthostatic headaches either. Thus, all CSF leaks do not cause headache.”
“Mechanism through which CSF leaks cause hearing changes via endolymphatic hydrops(Michel and Brusis, 1992). This diagram shows the general idea but it is inaccurate as there are other pathways for CSF flow other than the cochlear aqueduct.”
How does Hydrocephalus cause dizziness and/or unsteadiness?
https://www.dizziness-and-balance.com/disorders/central/hydrocephalus.html
There are several possible sources:
- Stretching of central connections controlling the legs causes spasticity and difficult controlling leg motion
- Fluctuation of pressure in the spinal fluid can be transmitted to the inner ear
- Headache pain from hydrocephalus might trigger migraine associated vertigo.
Regarding the hearing symptoms, oddly enough, tinnitus and low frequency hearing loss also is found in persons with low CSF pressure. One would think that either there is some mistake in attributing hearing symptoms to these conditions, as tinnitus is a common human symptom, or a shared mechanism (such as Migraine), that accounts for some of the symptoms.
Trigeminal neuralgia: Pathology and pathogenesis
Trigeminal neuralgia: Pathology and pathogenesis including Tinnitus and Hyperacusis
https://academic.oup.com/brain/article/124/12/2347/455086
More recently recognized syndromes of compression-induced cranial nerve hyperactivity include superior oblique myokymia due to vascular compression of the root entry zone of the trochlear nerve (Samii et al., 1998); `vestibular paroxysmia’ (Brandt and Dieterich, 1994), hyperacusis and tinnitus, due to vascular compression of the vestibulocochlear nerve in the cerebellopontine angle (Jannetta, 1977; Lesinski et al., 1979; Jannetta et al., 1986; Moller et al., 1993; Brandt and Dieterich, 1994; Ryu et al., 1998a; Okamura et al., 2000); geniculate neuralgia, due to vascular compression of the nervus intermedius (Lovely and Jannetta, 1997); spontaneous gagging and dysphagia due to vascular compression of the vagus adjacent to the medulla (Resnick and Jannetta, 1999); and spasmodic torticollis associated with vascular compression of the cranial accessory nerve close to the medulla (Pagni et al., 1985; Saito et al., 1993; Jho and Jannetta, 1995). In a significant proportion of patients with vascular compression of cranial nerve roots, multiple syndromes of cranial nerve hyperactivity are present in combination (Morales et al., 1977; Jamjoom et al., 1990; Kobata et al., 1998; Ryu et al., 1998b; Van et al., 1999).
https://en.wikipedia.org/wiki/Trigeminal_nerve
https://www.internetmedicin.se/page.aspx?id=3375
Increased risk of tinnitus following a trigeminal neuralgia diagnosis: a one-year follow-up study
https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-020-01121-6
Tinnitus due to hyperactivity across neuronal ensembles along the auditory pathway is reported. We hypothesized that trigeminal neuralgia patients may subsequently suffer from tinnitus. Using nationwide, population-based data and a retrospective cohort study design, we investigated the risk of tinnitus within 1 year following trigeminal neuralgia.
Tinnitus is the auditory phantom sensation of sound in the absence of external stimuli. About 10% of the population suffers from tinnitus, making it one of the most common health conditions in the world [1, 2]. The most common cause of tinnitus is tinnitus associated with hearing loss caused by noise overexposure and aging. However, tinnitus can result from non-otologic causes, such as head and neck trauma [3], temporomandibular disorders [4,5,6,7], and cervical spine disorders [8, 9]. A certain percentage of patients find their tinnitus provoked by movement of or applying pressure to the head and neck region [10, 11]. Research has shown that the somatic origins of tinnitus may be due to interactions between somatic and auditory neuronal pathways in the central nervous system, indicating the role of somatosensory components in some cases of tinnitus [10, 12,13,14,15,16].
Increased risk of tinnitus following a trigeminal neuralgia diagnosis: a one-year follow-up study
“Disruptions of the trigeminal nerve caused by neuralgia may also induce or contribute to tinnitus by affecting the vasculature of the inner ear. The trigeminal nerve is the source of innervation for blood vessels around the spiral modiolus and the stria vascularis of inner ear [31, 38].” https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-020-01121-6 & https://www.researchgate.net/publication/341201217_Increased_risk_of_tinnitus_following_a_trigeminal_neuralgia_diagnosis_a_one-year_follow-up_study
Swedish
Tinnitus och funktionsnedsättning I en käkmuskel https://www.diva-portal.org/smash/get/diva2:901204/FULLTEXT01.pdf Measuring EMG
Auditory nerve compression: a forgotten treatable cause for tinnitus
https://jnnp.bmj.com/content/81/4/355
Tinnitus has many causes, but it is most commonly related to hearing loss. Unfortunately, the tinnitus percept is generally not affected by conventional or high-bandwidth amplification (=hearing aids),1 and pharmacological treatment is unsuccessful in the majority of cases. Consequently, tinnitus is notoriously considered to be intractable to any form of treatment, resulting in the appearance of dramatic treatment approaches in the previous century such as prefrontal leucotomies, auditory nerve transsections and the recent development of brain stimulation techniques, in an attempt to reduce the defaitistic adagio: ‘you have to learn to live with it’.
There is, however, an almost unknown entity of vascular contact/compression of the …
Hyperactivity in the auditory brain follows cochlear damage?
Neural Hyperactivity of the Central Auditory System in Response to Peripheral Damage
https://www.hindawi.com/journals/np/2016/2162105/
“It is increasingly appreciated that cochlear pathology is accompanied by adaptive responses in the central auditory system. The cause of cochlear pathology varies widely, and it seems that few commonalities can be drawn. In fact, despite intricate internal neuroplasticity and diverse external symptoms, several classical injury models provide a feasible path to locate responses to different peripheral cochlear lesions. In these cases, hair cell damage may lead to considerable hyperactivity in the central auditory pathways, mediated by a reduction in inhibition, which may underlie some clinical symptoms associated with hearing loss, such as tinnitus. Homeostatic plasticity, the most discussed and acknowledged mechanism in recent years, is most likely responsible for excited central activity following cochlear damage.”
……
…. “7 Concluding remarks: Based on the research reviewed, it seems likely that specific insults to the peripheral auditory system, including cochlear ablation, selective IHC or OHC loss, and noise-induced mixed and incomplete IHC and OHC injuries, result in a reduction of input from the cochlea, thereby giving rise to hyperactivity in the central auditory circuits. A good example of this process is found in tinnitus, which may be associated with neuronal hyperactivity and is likely a common consequence of various kinds of cochlear damage. From an evolutionary perspective, hyperactivity in the brain may be a maladaptive response to reduced input, indicating that the system needs to become more sensitive to the reduced input to obtain more information and thereby remain balanced and stable. This dysfunctional neural state might contribute to some brain pathologies with auditory dysfunction, as indicated in a recent review suggesting that hyperactivity in the auditory brain is closely related to tinnitus and hyperacusis [110]. Despite these findings, it is still too early to say that hyperactivity in the auditory brain follows cochlear damage. Hopefully, a better understanding of altered neural properties in response to cochlear damage will provide new insights into the mechanism of injury-induced central plasticity, suggesting novel strategies for therapies.”
More is to come …
Middle Ear Myoclonus
(See also link ”hyperacusis and Stapendius muscle ….” informative text/pictures!)
Understanding How Middle Ear Myoclonus Causes Tinnitus – https://www.tinnitusformula.com/library/understanding-how-middle-ear-myoclonus-causes-tinnitus/ “Myoclonus refers to the spasmodic jerky contraction of a muscle or group of muscles. Hiccups are a form of myoclonus. In the middle ear, myoclonus can occur in the very small muscles behind the eardrum and in front of the cochlea.
There are two such muscles in the middle ear. The tensor tympani muscle attaches to the malleus bone in back of the eardrum. The stapedius muscle attaches to the stapes bone, that conducts sound to the cochlea. Both of these muscles are protective. They act to dampen sound levels coming into the ear and to reduce the sound of chewing and our own voice.
In the illustration below, the tensor tympani is the long dark muscle connected to the malleus bone inside the eardrum. The stapedius is the short red muscle attached to the stapes bone, the horseshoe shaped object.
Cartoon of the middle ear showing muscles that attach to ossicles (ear bones), and ear drum. The stapedius is attached to the stapes (of course — horseshoe object above), while the tensor tympani is attached to the ear drum. While useful, be aware that there are multiple errors in this illustration from Loyola Medical School. With permission, from: https://www.meddean.luc.edu/lumen/meded/grossanatomy/dissector/mml/images/stap.jpg
When the tensor tympani muscle is in spasm, it creates a thumping sound like a tympani drum. It can also be heard as a clicking sound. The thumping or clicking can produce a frequency as high as 90-100 times per minute. A doctor can actually see the eardrum vibrating and can hear the sound from 10-20 cm away.
When the stapedius muscle is in spasm is usually heard as a buzzing, rumbling or crackling sound. It cannot be observed affecting the eardrum but can sometimes be heard outside the ear.
MEM is quite rare, occurring in only about 6 in 10,000 people. But it can be maddening to have the thumping, clicking or buzzing sounds that will not stop. Causes of MEM include being subject to loud sounds such as artillery fire or nearby firecracker explosion. Stress can also bring it on. It can be caused by spasm in the facial nerve or the palate. When spasms start, they can often include both ears. Stress can play a major role, increasing the discomfort of the spasms.
Treatment of TT myoclonus that may work. https://www.dizziness-and-balance.com/disorders/hearing/tinnitus/tensor%20tympani%20and%20stapedius%20myoclonus%20tinnitus.html “Surgery to cut the muscle is effective, and is used as a last resort. According to Bhimrau et al (2012), the facial nerve is often damaged during this sort of surgery. However, it is generally successful in stopping the myoclonus. A recent report suggested using Botox to paralyze the muscles (Liu et al, 2011). Botox can be injected into the wall of the eustachian tube. Of course, the TT is a small muscle and thus only a small amount of Botox is needed (Botox, sold by Allergan, is extremely expensive). This treatment seems reasonable, except that one needs an individual to administer the Botox who has a very good understanding of the anatomy of the TT to administer the injection, and also Botox wears off in 3 months. Treatment of these muscle spasm syndromes is usually reassurance. Tinnitus coping strategies of counselling, relaxation and anxiety reduction are standard practice. Hypnosis, sedatives, psychotherapy, acupuncture, biofeedback have been attempted — as this type of tinnitus is somewhat related to stress, these strategies are sometimes helpful”.
Eardrum spasm https://www.healthline.com/health/eardrum-spasm#spasm The tensor tympani and stapedius muscles in your middle ear are protective. They dampen the sound of noises coming from outside the ear, and they reduce the sound of noises coming from the inside the body, such as the sound of our own voice, chewing, and so on. When these muscles spasm, the result can be middle ear myoclonus (MEM), also known as MEM tinnitus. MEM is a rare condition — occurring in about 6 of 10,000 people — in which tinnitus (buzzing or ringing in ears) is produced by repetitive and synchronized contractions of the tensor tympani and stapedius muscles.
The tensor tympani muscle attaches to the malleus bone — a hammer shaped bone that transmits sound vibrations from the eardrum. When it spasms, it makes a thumping or clicking sound.
The stapedius muscle attaches to the stapes bone, which conducts sound to the cochlea — a spiral-shaped organ in the inner ear. When it’s in spasm, it makes a buzzing or crackling sound.
According to a 2012 reviewTrusted Source of case reports and case series, there is no conclusive diagnostic test or treatment for MEM. Surgery on the stapedius and tensor tympani tendons (tenotomy) has been used for treatment — with varying degrees of success — when more conservative treatments have failed. A 2014 clinical study suggests an endoscopic version of this surgery as a possible therapeutic option. First-line treatment typically includes: muscle relaxants, anticonvulsants, zygomatic pressure. Botox treatment has been used as well.”
Menieres disease due to middle ear muscles behaving badly – https://lmhofmeyr.co.za/menieres-disease-due-middle-ear-muscles-behaving-badly/ “Meniere’s disease (MD) may well be caused by middle ear muscles behaving badly. This debilitating inner ear disease is characterized by episodes of vertigo, hearing loss, tinnitus and ear fullness of which the trigger is still unknown. The concept of endolymphatic hydrops (raise in the fluid pressure of the inner ear) is commonly accepted to be the explanation of what occurs in the inner ear, regardless of the trigger”.
“A new interesting theory has lately been advocated. The explanation is that the pressure in the inner increases (endolymphatic hydrops) may occur due to the inappropriate and abnormal contraction of the middle ear muscles, in particularly the tensor tympani muscle. Two of the smallest muscles in the human body are found in the middle ear. The stapedial muscle connects to the stapes (stirrup) and contraction with tilting of the stapes occurs reflexively to loud sound, protecting the inner ear to noise induced damage. The tensor tympani muscle on the other hand reacts to a lot of different triggers, such as the patient’s own voice, chewing and swallowing and also aim to protect the inner ear to sound. When the tensor tympani contracts the stapes is forced inwards. Momentarily it protects the inner ear by dampening the sound. Abnormal sustained contraction of the tensor tympani muscle with sustained inward displacement of the stapes unfortunately causes sustained increased inner ear pressure with compression of the outer hair cells and the generation of the symptoms of MD. Why this abnormal and often sustained muscle contraction (dystonia) occurs is not known.
If indeed future research shows that the middle ear muscles are to blame a logic approach would be to medically or surgically reduce the contraction. Care should be taken into making a decision on treatment as cutting or paralyzing the muscle may lead to other problems such as hypersensitivity to noise and hearing loss.”
8 causes of fluttering in the ear – https://www.medicalnewstoday.com/articles/fluttering-in-ear
“Fluttering in the ear is not typically a serious condition. However, it can affect a person’s quality of life and their ability to hear clearly.
How serious it is depends on the cause. People who experience fluttering in the ear may describe the sound as having helicopter blades or butterflies flapping their wings in their ear.
Diagnosing fluttering in the ear can be challenging for doctors, since guidelines for this do not yet exist. They will usually refer to published case reports to determine how to describe, diagnose, and treat fluttering in the ear.
Some people may experience clicking or buzzing sounds. Others may describe the sounds as: throbbing, tapping, crackling, bubbling, ticking, twitching, blowing, drum-like thumping, fluttering, whooshing, gushing.
People may hear the sounds in one or both ears, and the sounds may be: rhythmic, regular, irregular, continuous, intermittent
Some causes of tinnitus include dysfunctions in the ear, such as tumors and Meniere’s disease. Other causes include hearing loss and exposure to loud noises.
Middle Ear Myoclonus: Two Informative Cases and a Systematic Discussion of Myogenic Tinnitus – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3629860/ “…. Discussion: Both individual patient care and further elucidation of MEM will rely on more detailed clinical characterization as well as multidisciplinary input from neurology, otolaryngology, and dentistry.”
Middle ear myoclonus (MEM) syndrome – https://lmhofmeyr.co.za/conditions/middle-ear-myoclonus-mem-syndrome/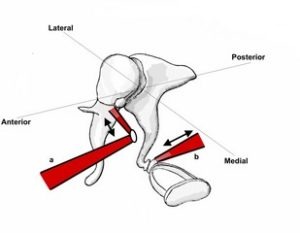
The middle ear muscles. a Tensor tympani muscle. b Stapedius muscle.
The middle ear contains muscles namely the stapedius muscle and the tensor tympani muscle. They attach to different ear bones( ossicles) and are innervated by separate cranial nerves. The function of the stapedius muscle is to stiffen the ossicular chain at the level of the stapes and is likely to attenuate external sound in order to protect the cochlea. The tensor tympani muscle attaches to the malleus an by contracting stiffens the ossicular chain at the level of the malleus and tympanic membrane. This action leads to the attenuation of internal body sound generated when swallowing, chewing and talking. Another function of these muscles is to produce movements at the ossicular joints in order for the joints to stay healthy and work effectively in protecting the tympanic membrane against ambient pressure changes … In the majority of cases the cause is unknown. Anxiety plays a major role and is believed to lower the threshold for the occurrence of the muscle contractions. Other conditions that may be responsible for objective tinnitus and need to be excluded include abnormal blood vessels, atherosclerosis, vascular tumours such as paraganglioma and multiple sclerosis … Management of MEM syndrome … see link.
A last picture of
 https://www.slideshare.net/mamoon901/middle-ear-anatomy-73261009
https://www.slideshare.net/mamoon901/middle-ear-anatomy-73261009
Otoacoustic Emissions
Otoacoustic Emissions (OAEs – https://www.asha.org/public/hearing/Otoacoustic-Emissions/
Otoacoustic Emissions https://emedicine.medscape.com/article/835943-overview
The primary purpose of otoacoustic emission (OAE) tests is to determine cochlear status, specifically hair cell function. This information can be used to (1) screen hearing (particularly in neonates, infants, or individuals with developmental disabilities), (2) partially estimate hearing sensitivity within a limited range, (3) differentiate between the sensory and neural components of sensorineural hearing loss, and (4) test for functional (feigned) hearing loss. The information can be obtained from patients who are sleeping or even comatose because no behavioral response is required.
The normal cochlea does not just receive sound; it also produces low-intensity sounds called OAEs. These sounds are produced specifically by the cochlea and, most probably, by the cochlear outer hair cells as they expand and contract. The presence of cochlear emissions was hypothesized in the 1940s on the basis of mathematical models of cochlear nonlinearity. However, OAEs could not be measured until the late 1970s, when extremely sensitive low-noise microphones needed to record these responses became available.
The four types of OEAs are as follows:
Spontaneous otoacoustic emissions (SOAEs) – Sounds emitted without an acoustic stimulus (ie, spontaneously)
Transient otoacoustic emissions (TOAEs) or transient evoked otoacoustic emissions (TEOAEs) – Sounds emitted in response to acoustic stimuli of very short duration; usually clicks but can be tone-bursts
Distortion product otoacoustic emissions (DPOAEs) – Sounds emitted in response to 2 simultaneous tones of different frequencies
Sustained-frequency otoacoustic emissions (SFOAEs) – Sounds emitted in response to a continuous tone
More is to come …
The inner ear and the neurologist
Inner ear disorders are common and patients with vestibular failure often present to a neurology clinic because of their dizziness, gait unsteadiness and oscillopsia. Vestibular disorders can be divided into peripheral and central vestibular disorders. Most of the peripheral vestibular disorders have a clinical diagnosis, and a thorough history and examination will often provide a clear direction as to the diagnosis. Correct diagnosis allows treatment for many of the peripheral and central vestibular disorders. As inner ear damage is generally irreversible, early diagnosis allowing prompt treatment is important. The aim of this review is to discuss some audiovestibular conditions that may well appear in a neurology clinic, and to discuss some recent advances within the audiovestibular field that may be of interest to neurologists. Some of the most common audiovestibular conditions will be discussed along side more uncommon conditions. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2077664/
https://www.researchgate.net/publication/6572395_The_inner_ear_and_the_neurologist
The association between tinnitus, the neck and TMJ
https://mskneurology.com/association-tinnitus-neck-tmj/
“Tinnitus and other hearing disorders are often associated with specific musculoskeletal factors, and these may be treated with good results. The nerves that control the structures of the middle ear, such as the eustachian tube, ossicles and tympanic membrane may become entrapped within the neck or jaw, causing faulty signalling to the ear and thus varying degrees of dysautonomia, which may in turn result in hearing and vestibular disorders. It is therefore important to examine these structures before prematurely concluding that the cause of the disorder must be vestibulocochlear nerve dysfunction or idiopathic hair cell destruction.
Furthermore, endolymphatic regulation in the inner ear may be disturbed both by nervous entrapment in the same regions, as well as impaired venous drainage. Sometimes also by compromised arterial supply, although a little less common. The most common endolymphatic pathology is excessive endolymphatic fluid, which may cause ischemia of the stria vascularis as well as destruction of the stereocilia (hair cells) of the main hearing organ (the organ of Corti). Buildup of endolymph has been demonstrated even when the stria vascularis is damaged (which produces endolymph), indicating that impaired drainage is the most likely culprit. In line with this, patients who have been shown to develop endolympathic hydrops, also also have a very high prevalence of migraines, which has been correlated with venous restrictions as well. It is thus likely that endolymphatic hydrops (or ‘mere’ excess) is caused by a combination of poor neural regulation (possibly due to entrapment), as well as venous outflow restrictions.
In most circumstances, multiple factors contribute to the hearing disorders, and many of these can be treatable. This can in most cases lead to improvement of the disorder, and sometimes also lead to complete reversal.
Technically, the main structures to be aware of, are the trigeminal and vagus nerves, as well as the cervical sympathetic plexus and Cruveilhier’s plexus, which may become entrapped in the neck and jaw, causing diffuse symptoms, often of aural nature. The internal jugular vein may become compressed by neck hinging or atlas torsion, causing restricted outflow, as the tympanic complex’ veins drain into the sigmoid sinus, which in turn drain into the jugular vein.”
Cochlea Migraine (without headache)
https://www.neurologylive.com/view/new-category-migraine – “In this large-scale cohort study, we found that patients with a history of migraine had a tendency to develop cochlear disorders, especially tinnitus, defined in one study as ”the perception of a sound with a lack of an evident external stimulus to that sound.”2 The results of this study supported the new concept and/or presence of cochlear migraine,” wrote first author Juen-Haur Hwang, MD, PhD, of Tzu Chi University (Hualien, Taiwan), and colleagues.
While many patients with migraine have headaches, symptoms of migraine can also occur without head pain and can affect vision, hearing, smell, and touch. Hyperacusis, or increased sensitivity to sound, can be a symptom of migraine that is also associated with disorders of the cochlea, which is found in the inner ear. But whether migraine is associated with cochlear disorders has been unclear.”
NB Migraine without headache but not mentioning Tinnitus:
Silent Migraine: A Guide https://americanmigrainefoundation.org/resource-library/silent-migraine/ also https://www.webmd.com/migraines-headaches/what-are-silent-migraines as well as https://health.clevelandclinic.org/a-migraine-without-pain-yes-it-can-happen-and-its-called-an-ocular-migraine/ and https://www.medicalnewstoday.com/articles/324890
Tinnitus and Headache
https://americanmigrainefoundation.org/resource-library/understanding-migrainetinnitus-and-headache/
https://www.eyeandear.org.au/page/Patients/Patient_information/Balance_Disorders/What_are_some_types_of_balance_disorders/Vestibular_migraine/
https://www.migrainestrong.com/the-tinnitus-and-migraines-link-simple-strategies-to-tune-it-out/
https://www.tinnitus.org.uk/blog/do-headaches-make-tinnitus-worse
https://migraine.com/blog/tinnitus/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5581323/
Cochlea and Tinnitus
Functional Anatomy of the Human Cochlear Nerve and Its Role in Microvascular Decompressions for Tinnitus https://academic.oup.com/neurosurgery/article-abstract/54/2/381/2740051 “The functional anatomy (i.e., tonotopy) of the human cochlear nerve is unknown. A better understanding of the tonotopy of the central nervous system segment of the cochlear nerve and of the pathophysiology of tinnitus might help to ameliorate the disappointing results obtained with microvascular decompressions in patients with tinnitus …. Conclusion: The tonotopic organization of the cisternal segment of the cochlear nerve has an oblique rotatory structure as a result of the rotatory course of the cochlear nerve in the posterior fossa. Knowledge of this tonotopic organization of the auditory nerve in its cisternal course might benefit surgeons who perform microvascular decompression operations for the vestibulocochlear compression syndrome, especially in the treatment of unilateral severe tinnitus”.
Text and pictures coming …
Two main pathways from Cochlea
”.. Two main cochlear pathologies could be at the origin of tinnitus: malfunction of the glutamatergic synapse between the inner hair cell and the auditory nerve, and the disruption of the outer hair cells’ active mechanisms” http://www.cochlea.eu/en/pathology/tinnitus
Below a second two pathways picture; “Figure 5. Schematic diagram of the auditory projections in the brain. The “classical” auditory pathway conveying information about sound from the ear to the cortex is shown by the green arrows. The other projections from the auditory system to structures relating to emotion and arousal are shown with the red arrows. General descriptors of function in these structures are included in red text. https://www.researchgate.net/figure/The-human-auditory-system-A-cross-section-of-the-ear-B-Cross-section-of-the-cochlear_fig5_320077050
Below you can see how the above shown non-specific pathways approach the Reticular Activation Systems and then proceed …
More text coming …
 https://integratedlistening.com/meet-the-reticular-activating-system-ras/
https://integratedlistening.com/meet-the-reticular-activating-system-ras/
The above picture is more discussed together with Orienting Responses and Habituation. A complex matter which can be a prat of extreme severe multifaceted Tinnitus
An other picture; Components of the Auditory Pathway

GABA and Glutamate – neurotransmittor imbalance
Link provider of GABA supplements refers to https://www.healthline.com/health/gamma-aminobutyric-acid#side-effects
- GABA receptor in the medial temporal lobe, and it inhibits central nervous system synapse activity. But GABA glitches can lead to convulsions. This correlation provides clinical support for a new theory that proposes tinnitus is an epileptic-like auditory phenomenon. According to this theory, overly excitable nerve cells instigate both epilepsy and tinnitus. Healthy nerves automatically shut down nerve signaling when they get too excited. GABA (gamma-aminobutyric acid) is an amino acid and the brain’s primary inhibitory neurotransmitter. When GABA transmitters are working properly, they act like a brake on overstimulated neurons by blocking glutamate, the principle excitatory transmitter. But in some brains, this system malfunctions, and the nerves continue to fire off signals, overloading the system and triggering seizures (epilepsy) or phantom ringing (tinnitus). Researchers have found that GABA receptor deficiencies may aggravate tinnitus. Scans from single-photon emission computed tomography (SPECT) show decreased chemical binding and other GABA-receptor irregularities in those suffering severe tinnitus …” .. Two main cochlear pathologies could be at the origin of tinnitus: malfunction of the glutamatergic synapse between the inner hair cell and the auditory nerve, and the disruption of the outer hair cells’ active mechanisms” http://www.cochlea.eu/en/pathology/tinnitushttps://www.frontiersin.org/articles/10.3389/fnins.2018.00866/full
- ”.. Sites of Tinnitus Generation – … “Zenner (1998) initially postulated that tinnitus could originate in any relevant anatomical structure; from the ear throughout the central auditory pathways” .. .. “Peripheral tinnitus” refers to the auditory perception that results from aberrant neural activity at the cochlear level and transmitted through the auditory pathways”
- ” Researchers have known for many years that high-level noise induces oxidative stress in the cochlea. It does this by causing a decrease in blood flow, releasing excessive amounts of glutamate, a toxic excitatory neurotransmitter, and stressing the mitochondria. Oxygen free radicals are thereby generated in the cochlea. Free radicals are toxic to the hair cells and neurons in the auditory pathway. (1 – https://www.audiologyonline.com/interviews/interview-with-richard-kopke-m-1447) … There are over 200 ototoxic medications, both prescription and over-the-counter, that can damage hearing and cause tinnitus. The mechanism of action seems to be similar to that of noise trauma; the drugs potentiate glutamate receptors in the cochlea that promote degradation of hair cells and neurons. This in turn leads to a cascade of free radicals, which further destroys the hair cells and neurons
- … “When GABA transmitters are working properly, they act like a brake on overstimulated neurons by blocking glutamate, the principle excitatory transmitter””Glutamate controls communication between auditory centers in the brain and the inner hair cells of the cochlea. When these hair cells become damaged by things like exposure to loud noise or ototoxic substances, excessive glutamate is released. Glutamate exhibits neurotoxic properties in excessive amounts or when inadequately recycled. This malfunction leads to excitotoxicity and can cause neuronal death of auditory nerves. Too much glutamate opens neuronal sodium channels and stops them from closing, causing the neurons to keep firing.There are two basic ways to correct this imbalance.
(a) “Activate GABA receptors to stop glutamate-induced firing. Anti-anxiety supplements that activate GABA receptors can help regulate glutamate levels and protect mitochondria from instigating cell death”
(b) Avoid food and other substances that contain excitotoxins – especially monosodium glutamate (MSG). MSG is a highly concentrated salt form of glutamic acid linked to multiple health problem that can exacerbate tinnitus. And avoid oxotoxic chemicals and substances that can interfere with proper neurotransmission and cause excess glutamate to build up in the brain.Protecting the blood-brain barrier and ensuring proper cerebral blood flow can further protect neuronal cells from cell death and may help reduce symptoms of tinnitus. Nootropics for tinnitus can improve cerebral blood flow and oxygen for better protection.” ““Researchers have found that GABA receptor deficiencies may aggravate tinnitus” https://www.mindlabpro.com/blogs/nootropics/nootropics-tinnitus“Activate GABA receptors to stop glutamate-induced firing. Anti-anxiety supplements that activate GABA receptors can help regulate glutamate levels and protect mitochondria from instigating cell death” ““Researchers have found that GABA receptor deficiencies may aggravate tinnitus” https://www.mindlabpro.com/blogs/nootropics/nootropics-tinnitus - GABAa – Benzodiazepine-Chloride Receptor-Targeted Therapy for Tinnitus Control:
https://pdfs.semanticscholar.org/4841/d6dbacde4e19a5f2ff9d6f487961f3d29c83.pdf
“Treatment options were presented to patients prior to RTT and included instrumentation; medication (e .g., pentoxifylline); treatment of factors known to be identified with development or continuation of severe disabling tinnitus (i.e ., fluctuation in aeration of the middle ears bilaterally; secondary endolymphatic hydrops); and control of noise exposure.Developmental Deficits in GABA Lead to Abnormal Brain Rhythms in Sensory Areas https://news.weill.cornell.edu/news/2020/01/developmental-deficits-in-gaba-lead-to-abnormal-brain-rhythms-in-sensory-areas”Decreased amounts of a neurotransmitter called GABA, whose main function is to reduce activity in the brain, leads to changes in the number of neurons in the developing brain and alters signaling between them, according to new research by Weill Cornell Medicine investigators. The findings could lead to an improved understanding of autism and sensory processing disorders (BvS including different kinds of Tinnitus).There are two kinds of neurons in the cortex: Excitatory neurons “fire” and pass signals on to other neurons and inhibitory neurons—interneurons—stop signals from being transmitted through the nervous system. In mammals, the nervous system matures during early life, establishing a balance of the two kinds of neurons. Alterations in the way neurons connect or communicate with one another during this period can affect long-term cognitive and behavioral responses.”
… Much more is to come here as well as how I have done myself
Hair cells – outer and inner functions
“Inner ear disorders include: Acoustic neuroma, Benign paroxysmal positional vertigo, Drug-induced ototoxicity, Herpes zoster oticus, Meniere disease, Purulent labyrinthitis and Vestibular neuronitis”. https://www.msdmanuals.com/professional/ear-nose-and-throat-disorders/inner-ear-disorders/introduction-to-inner-ear-disorders
The outer hair cells mechanically amplify low-level sound that enters the cochlea.[6][7] The amplification may be powered by the movement of their hair bundles, or by an electrically driven motility of their cell bodies. This so-called somatic electromotility amplifies sound in all land vertebrates. It is affected by the closing mechanism of the mechanical sensory ion channels at the tips of the hair bundles.[citation needed]
The inner hair cells transform the sound vibrations in the fluids of the cochlea into electrical signals that are then relayed via the auditory nerve to the auditory brainstem and to the auditory cortex.
https://en.wikipedia.org/wiki/Hair_cell#Outer_hair_cells_%E2%80%93_acoustical_pre-amplifiers
Inner Ear Hair Cell Protection in Mammals against the Noise-Induced Cochlear Damage https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6079343/
Inner ear hair cells are mechanosensory receptors that perceive mechanical sound and help to decode the sound in order to understand spoken language. Exposure to intense noise may result in the damage to the inner ear hair cells, causing noise-induced hearing loss (NIHL). Particularly, the outer hair cells are the first and the most affected cells in NIHL. After acoustic trauma, hair cells lose their structural integrity and initiate a self-deterioration process due to the oxidative stress.
The activation of different cellular death pathways leads to complete hair cell death. This review specifically presents the current understanding of the mechanism exists behind the loss of inner ear hair cell in the auditory portion after noise-induced trauma. The article also explains the recent hair cell protection strategies to prevent the damage and restore hearing function in mammals.
” A recent work of Fuentes-Santamaría et al. also determined the permanent hearing threshold shift in response to loud noise overexposure. This shift simultaneously occurred with the outer hair cell loss, upregulation of prestin, and microglial activation. The authors also observed that the TNF-α and interleukin 1β were upregulated by the microglia, fibrocytes, and neuronal cells at different time points in the noise-exposed cochlea [43] suggesting that there is an involvement of complex interplay among the different cytokine-producing cells that might be responsible for cochlear pathophysiology in the noiseexposed cochlea” … “recent studies also highlight that the synapse degeneration in the inner ear is another key contributor of NIHL. The synapsis between the inner hair cells and spiral ganglion neurons is more prone to cellular damage [65].
Glutamate excitotoxicity and calcium signaling pathways are considered as a candidate in cochlear synaptopathy. The excessive release of glutamate results in a synaptic destruction between inner hair cells and spiral ganglion neurons [66]. This excessive glutamate concentration further leads to the huge influx of calcium, sodium, and potassium ions into the spiral ganglion neurons that ultimately swell and damage the synaptic structures [67–69].
Moreover, L-type and T-type calcium channels also participated to excessive calcium influx after noise-induced damage [70, 71]. However, the role of different signaling pathways and the exact mechanism of cochlear synaptopathy are not completely understood yet and need further investigations in the future”.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6079343/pdf/NP2018-3170801.pdf
Some “function possibilities” to be considered Static length changes of cochlear outer hair cells can tune low-frequency hearing – https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1005936
The cochlea not only transduces sound-induced vibration into neural spikes, it also amplifies weak sound to boost its detection. Actuators of this active process are sensory outer hair cells in the organ of Corti, whereas the inner hair cells transduce the resulting motion into electric signals that propagate via the auditory nerve to the brain. However, how the outer hair cells modulate the stimulus to the inner hair cells remains unclear. Here, we combine theoretical modeling and experimental measurements near the cochlear apex to study the way in which length changes of the outer hair cells deform the organ of Corti. We develop a geometry-based kinematic model of the apical organ of Corti that reproduces salient, yet counter-intuitive features of the organ’s motion. Our analysis further uncovers a mechanism by which a static length change of the outer hair cells can sensitively tune the signal transmitted to the sensory inner hair cells. When the outer hair cells are in an elongated state, stimulation of inner hair cells is largely inhibited, whereas outer hair cell contraction leads to a substantial enhancement of sound-evoked motion near the hair bundles. This novel mechanism for regulating the sensitivity of the hearing organ applies to the low frequencies that are most important for the perception of speech and music. We suggest that the proposed mechanism might underlie frequency discrimination at low auditory frequencies, as well as our ability to selectively attend auditory signals in noisy surroundings”.
Modulation of hair cell efferent
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3125486/
“Outer hair cells (OHCs) amplify the sound-evoked motion of the basilar membrane to enhance acoustic sensitivity and frequency selectivity. Medial olivocochlear (MOC) efferents inhibit OHCs to reduce the sound-evoked response of cochlear afferent neurons. OHC inhibition occurs through the activation of postsynaptic α9α10 nicotinic receptors tightly coupled to calcium-dependent SK2 channels that hyperpolarize the hair cell. MOC neurons are cholinergic but a number of other neurotransmitters and neuromodulators have been proposed to participate in efferent transmission, with emerging evidence for both pre- and postsynaptic effects. Cochlear inhibition in vivo is maximized by repetitive activation of the efferents, reflecting facilitation and summation of transmitter release onto outer hair cells. This review summarizes recent studies on cellular and molecular mechanisms of cholinergic inhibition and the regulation of those molecular components, in particular the involvement of intracellular calcium. Facilitation at the efferent synapse is compared in a variety of animals, as well as other possible mechanisms of modulation of ACh release. These results suggest that short-term plasticity contributes to effective cholinergic inhibition of hair cells.”
Targeting inhibitory neurotransmission in tinnitus https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3374875/
“Tinnitus perception depends on the presence of its neural correlates within the auditory neuraxis and associated structures. Targeting specific circuits and receptors within the central nervous system in an effort to relieve the perception of tinnitus and its impact on one’s emotional and mental state has become a focus of tinnitus research. One approach is to upregulate endogenous inhibitory neurotransmitter levels (e.g. glycine and GABA) and selectively target inhibitory receptors in key circuits to normalize tinnitus pathophysiology. Thus, the basic functional and molecular properties of two major ligand-gated inhibitory receptor systems, the GABAA receptor (GABAAR) and glycine receptor (GlyR) are described. Also reviewed is the rationale for targeting inhibition which stems from reported tinnitus-related homeostatic plasticity of inhibitory neurotransmitter systems and associated enhanced neuronal excitability throughout most central auditory structures. However, the putative role of the medial geniculate body (MGB) in tinnitus has not been previously addressed, specifically in terms of its inhibitory afferents from inferior colliculus and thalamic reticular nucleus and its GABAAR functional heterogeneity. This heterogeneous population of GABAARs, which may be altered in tinnitus pathology, and its key anatomical position in the auditory CNS make the MGB a compelling structure for tinnitus research. Finally, some selective compounds, which enhance tonic inhibition, have successfully ameliorated tinnitus in animal studies, suggesting that the MGB and, to a lesser degree, the auditory cortex may be their primary locus of action. These pharmacological interventions are examined, in terms of their mechanism of action and why these agents, may be effective in tinnitus treatment”.
Cochlear hair cells: The sound-sensing machines – https://www.sciencedirect.com/science/article/pii/S0014579315007309
The sensory epithelium of the mammalian inner ear contains two types of mechanosensory cells: inner (IHC) and outer hair cells (OHC). They both transduce mechanical force generated by sound waves into electrical signals. In their apical end, these cells possess a set of stereocilia representing the mechanosensing organelles. IHC are responsible for detecting sounds and transmitting the acoustic information to the brain by converting graded depolarization into trains of action potentials in auditory nerve fibers. OHC are responsible for the active mechanical amplification process that leads to the fine tuning and high sensitivity of the mammalian inner ear. This active amplification is the consequence of the ability of OHC to alter their cell length in response to changes in membrane potential, and is controlled by an efferent inhibitory innervation. Medial olivocochlear efferent fibers, originating in the brainstem, synapse directly at the base of OHC and release acetylcholine. A very special type of nicotinic receptor, assembled by α9α10 subunits, participates in this synapse. Here we review recent knowledge and the role of both afferent and efferent synapse in the inner ear”
Fig 1. “Course of the medial and lateral efferent system. A, The auditory brainstem section. Sound representations from the ear ascend to the olivary complex via the ventral afferent pathway and project back to the ear via dorsal crossed and uncrossed medial and lateral efferent fibers. B Cross-sectional view of the inner ear. The major ascending afferent pathway arises from inner hair cells. Descending olivocochlear projections terminate on inner and outer hair cells. (with permission from Liberman MC. Effects of chronic cochlear de-differentiation on auditory-nerve response. Hear Res 1990; 49: 209–224, © 1990, Elsevier; and May BJ, Budelis J, Niparko JK. Behavioral studies of the olivocohlear efferent system. Arch Otolaryngol Head Neck Surg 2004; 130: 660–664; Copyright © 2004, American Medical Association. All rights reserved).”
Cochlear Outer Hair Cell Motility https://www.uclahealth.org/head-neck-surgery/workfiles/Secure/OHC_Motility-Ashmore_Review08.pdf
Microchondria and Tinnitus
First a very comprehensive general (not specifically for Tinnitus) overview – Our (Mother’s) Mitochondria and Our Mind https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5761714/
Then a picture
 https://www.tinnitusformula.com/mitochondria/
https://www.tinnitusformula.com/mitochondria/
Tinnitus in patients with hearing loss due to mitochondrial DNA pathogenic variants – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6060765/ – “Purpose; Tinnitus described as individual perception of phantom sound constitutes a significant medical problem and has become an essential subject of many studies conducted worldwide. In the study, we aimed to examine the prevalence of tinnitus among Polish hearing loss (HL) patients with identified mitochondrial DNA (mtDNA) variants. Conclusion: Our data suggest that the mtDNA variants causative of HL may affect tinnitus development but this effect seems to be ethnic-specific.”
The role of mitochondrial oxidative stress in hearing loss
https://www.oatext.com/the-role-of-mitochondrial-oxidative-stress-in-hearing-loss.php#gsc.tab=0
“.. Hearing impairment following cochlear damage due to noise trauma, ototoxicity or age‐related cochlear degeneration was linked to a common pathogenesis involving the formation of reactive oxygen species (ROS). This review summarizes the current data suggesting a role of mitochondrial ROS overproduction in hearing loss and the molecular mechanism involved in hair cell apoptosis responsible of this disorder. Because increasing number of studies demonstrated that antioxidants and free radical scavengers may serve as effective compounds to block the activation of cochlear hair cell death, targeting members of antioxidant pathways and in the breakdown of superoxide anions and hydrogen peroxidase, could be feasible options for the treatment of several types of hearing loss”.
Hightlight
– ROS overproduction plays a key role in hearing loss
– ROS induce mitochondrial damage and cochlear hair cell apoptosis
– Antioxidants as effective therapeutic agents for hearing disorders
2.1. Noise-Induced Oxidative Stress https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6079343/
The reactive oxygen species (ROS) are observed in the hair cells after the acoustic overexposure and exist there for about 10 days [25]. The ROS are produced in the cell mitochondria, and disturbance in the integrity of mitochondria may result in the production and continuous release of ROS in the cell cytoplasm [26, 27]. The generation of reactive oxygen species and the increased metabolic activity in the hair cells after noise-induced ototoxicity have been reported to create hair cell loss (Figure 1) [28–31]. The reactive nitrogen species (RNS) also accumulate in the hair cells after being exposed to loud voices [32, 33]. Both the ROS and RNS have stimulated caspase-mediated apoptotic cell death pathways in the cochlea [30, 34]. Besides, ROS formation also promotes inflammation and generates proinflammatory cytokines such as interleukin (IL) 6 and [35, 36], tumor necrosis factor-α (TNF-α)”
See also headlines in this link head lines as
“2.2. Caspase- and JNK-Dependent Hair Cell Death Pathways
2.3. Caspase-Independent Cell Death Pathway
2.4. Excessive Calcium Accumulation in Hair Cells
- Strategies for Hair Cell Protection in Mammals against the Noise-Induced Hearing Loss
…
As well as Conclusion; In recent years, research on the noise-induced hearing loss is focused in order to develop various therapeutic strategies for appropriate protection of hair cells from any damage and to restore the auditory function after acoustic trauma ….. “
Oxidative stress, nitric oxide, endothelial dysfunction and tinnitus – https://www.tandfonline.com/doi/abs/10.1080/10715760600623825 “To assess whether pathogenic endothelial dysfunction is involved in acute idiopathic tinnitus we enrolled 44 patients and 25 healthy volunteers. In blood from the internal jugular vein and brachial vein we determined malonaldehyde, 4-hydroxynonenal, mieloperoxidase, glutathione peroxidase, nitric oxide, l-arginine and l-ornitine, thrombomodulin (TM) and von Willebrand factor (vWF) activity during tinnitus and asymptomatic period.
Higher plasma concentrations of oxidative markers and l-arginine, and lower nitric oxide and l-ornitine levels were observed in jugular blood of patients with tinnitus, there being a significant difference between brachial and jugular veins. TM and vWF activity were significantly higher in patients’ jugular blood than in brachial blood.
Our results suggest oxidant, TM, vWF activity production are increased and nitric oxide production reduced in brain circulation reflux blood of patients with acute tinnitus. These conditions are able to cause a general cerebro-vascular endothelial dysfunction, which in turn induce a dysfunction of microcirculation in the inner ear.”
Antioxidant Therapy in Idiopathic Tinnitus: Preliminary Outcomes – https://d1wqtxts1xzle7.cloudfront.net/46597224/j.arcmed.2006.12.00420160618-27019-1q1ljx.pdf?1466265309=&response-content-disposition=inline%3B+filename%3DAntioxidant_Therapy_in_Idiopathic_Tinnit.pdf&Expires=1599652556&Signature=AeSoaPqRjpPyb-TTph3vZp6FVDLJj9XsJmemFy9Spcs8zRZ3fuKrCTZSXMLQoqtSUJn0R-v4GB~OWE3INN8bNFSplNUpQfvUA99Tx5bwgpKO0E4ze1PCDXfh-kubx83Q4G1yXLE~Nm5hk-8cPvnoMsybydD9juqhtlbtZ0mgODc8wmFxshnKlNzMMdZZxdWr2okJJnsnulZtorcJIw3T53kJsXlsM76H0ylTyu3znbR1X~EmWeQxhv7eQBW5JZ-sRzMSpzH9a-1t8H7CbJPA7pgNBZ9xqxBOPkoYQV7WoGprHNTPk3Km~3lVIqwUAu7xjKQNhAVQ6WsIxqSNlglvmw__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA “Background. Reactive oxygen species (ROS) play an important role in several pathogenic processes, damaging various structural and functional cellular components. The endothelium is at major risk of radical-induced lesions and this damage is most manifest in microcirculation. It has been recently observed that ROS are implicated in the pathology of the inner ear and the peripheral and central pathways. In a previous study we detected high serum values of ROS in subjects with idiopathic tinnitus. The purpose of the present study was to evaluate the validity of antioxidant treatment in tinnitus sufferers with high ROS values.
Methods. The study considered 31 consecutive patients with unilateral idiopathic tinnitus. The mean pure tone audiometric threshold (PTA), tinnitus loudness, subjective disturbance level [visual analogue scale (VAS) determination], and the indirect ROS
dosage 48 h before and after medical treatment were evaluated. Patients underwent an
18-week oral treatment with a mix of phospholipids and vitamins (glycerophosphorylcholine, glycerophosphorylethanolamine, b-carotene, vitamin C, vitamin E).
Results. ROS levels were significantly reduced following antioxidant treatment (malonaldehyde: 2.10 vs. 1.98 mmol/dL, p 5 0.003; 4-hydroxynonenal: 2.36 vs. 2.16 mmol/dL, p 5 0.002) In addition, great improvement was observed in the reduction of tinnitus (VAS and tinnitus loudness evaluations). No significant changes in audiometric threshold occurred.
Conclusions. Oral antioxidant therapy in patients with idiopathic tinnitus seems to
reduce the subjective discomfort and tinnitus intensity and may be considered as an additional treatment modality”
Microcirculation and Tinnitus
Physiopathology of the Cochlear Microcirculation – https://www.researchgate.net/publication/51603595_Physiopathology_of_the_Cochlear_Microcirculation “Normal blood supply to the cochlea is critically important for establishing the endocochlear potential and sustaining production of endolymph. Abnormal cochlear microcirculation has long been considered an etiologic factor in noise-induced hearing loss, age-related hearing loss (presbycusis), sudden hearing loss or vestibular function, and Meniere’s disease. Knowledge of the mechanisms underlying the pathophysiology of cochlear microcirculation is of fundamental clinical importance. A better understanding of cochlear blood flow (CoBF) will enable more effective management of hearing disorders resulting from aberrant blood flow. This review focuses on recent discoveries and findings related to the physiopathology of the cochlear microvasculature.”
Assessment of the effect of mesoglycan in the treatment of audiovestibular disorders of vascular origin https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5946343/ “It is a well-known fact that inner ear diseases are often caused by microcirculatory disorders, and the recent literature is oriented towards investigations into the relationship between the cardiovascular system and cochleovestibular illness with related classical symptoms: tinnitus, hearing loss, and vertigo or instability” … “The data collected showed that the treatment with mesoglycan, irrespective of the type of vascular risk factor, is not only well tolerated but also significantly and objectively improves the cochleovestibular symptoms and the quality of life of patients suffering from tinnitus, peripheral vertigo and instability”
Natural Solutions for Tinnitus – https://www.arc-nutrition.com/natural-solutions-for-tinnitus/ “…Tinnitus isn’t a condition itself, but instead a symptom of an underlying cause. Ear injury, age-related hearing loss, or a circulatory disorder can cause tinnitus to afflict the hearer. If the cause is circulatory, there are a few things you can attempt to naturally alleviate this symptom.
Boost Your Stem Cells – Endothelial progenitor cells (EPCs) are the stem cells naturally produced by your bone marrow, but that production starts to decline after the age of 25. This study on endothelial dysfunction and tinnitus concludes that conditions which cause a general endothelial dysfunction will in turn induce a dysfunction of the inner ear’s microcirculation: this is one of the underlying causes of tinnitus. EPCs are the repair-and-replace stem cells of the circulatory system, and have the ability to hone to areas of injury once they are released into the bloodstream. Luckily there are natural ways to increase your body’s production of EPCs, and relieve not only tinnitus, but the circulatory problems causing it.
Increase Healthy Circulation: Likewise, another natural way to alleviate tinnitus caused by circulatory issues is to improve blood flow to the inner ear. Pine bark extract or its concentrate Pycnogenol can increase vascular delivery to the affected ear in as little as two weeks. Results of increased circulation to the inner ear can include reduction of tinnitus, increased hearing, and improved balance with the treatment of vertigo.
With pine bark extract to help thin the blood and improve blood flow, that is another all-natural way to decrease or potentially eradicate it. Studies have also shown Pycnogenol’s potential to lower blood pressure, improve skin conditions, and ease Meniere’s disease symptoms including vertigo and hearing loss. Supplementing your daily regimen with pine bark extract can improve your circulation and your overall health.
With tinnitus: focus on the underlying cause, and you can potentially help the symptom.”
Transcutaneous Nerve Stimulation (TNS) in Tinnitus – https://www.tandfonline.com/doi/abs/10.3109/14992028909042196 “Low-frequency (2 Hz) TNS applied distally to peripheral nerves of the upper extremity is known to induce a widespread, non-segmental and prolonged relief of pain and an increased microcirculation due to sympatho-inhibition in a number of vascular beds. Such stimulation was administered in 29 tinnitus patients of various etiology. Reduction of tinnitus was encountered in 9 subjects in response to a 45-min TNS-session. The improvement was mainly seen in tinnitus characterized by lower frequencies (125–500 Hz). In 7 of the 9 patients, the tinnitus reduction was associated with improvement of hearing, predominantly in the low-frequency band. The effects were still present after one week following daily stimulation at home. On continued treatment, the effects were found to be transitory in 4 of the patients, whereas the remaining 5 patients are still using the stimulator after 2 to 5 years. It is suggested that the mechanism behind the beneficial effects is increased microcirculation in part of the auditory pathways”.
Audiological Tinnitus Management: An Essential Audiological Protocol for Elderly Patients with Comorbidity of Hypertension and Tinnitus – https://www.intechopen.com/books/management-of-tinnitus-the-enriching-views-of-treatment-options/audiological-tinnitus-management-an-essential-audiological-protocol-for-elderly-patients-with-comorb “Elderly population with comorbidity of hypertension and tinnitus is increasing across the world, and the dilemma in the management of such elderly patients across the neurology and audiology/otology clinics seems enormous due to the attendant effects of such health-related comorbid conditions and ageing. This has been observed to have negative effect on the general well-being of quite a number of the elderly patients identified with the comorbid health conditions. It has also increased the tinnitus severity and related psychosocial reactions of the elderly patients. Worse still, the situation causes undulating increase in the prevalence of the comorbid condition of advanced age both male and female irrespective of cultural differences. Due to the aforementioned, this chapter is written with the aim of highlighting the efficacy of audiological tinnitus management options considered essential in the rehabilitation of individuals with comorbidity of hypertension and tinnitus. The chapter also discusses the benefits of combined therapies in rehabilitating elderly patients with comorbidity of hypertension and tinnitus and concluded with some useful recommendations for effective management of the comorbid condition.
New 2020-09-24
GABAB receptors as drug targets to treat gastroesophageal reflux disease – https://pubmed.ncbi.nlm.nih.gov/19303900/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2275437/
https://www.jpeds.com/article/S0022-3476(06)00688-3/fulltext
Effect of acute and chronic administration of the GABAB agonist baclofen on 24 hour pH metry and symptoms in control subjects and in patients with gastro-oesophageal reflux disease – https://gut.bmj.com/content/52/4/464
New 2020-09-24
Gastroesophageal Reflux Disease (GERD) and Your Ears – https://hearinglosshelp.com/blog/gastroesophageal-reflux-disease-gerd-and-your-ears/
Here’s an alarming statistic. “The number of people hospitalized for conditions related to GastroEsophageal Reflux Disease (GERD) doubled between 1998 and 2005.” At the present time, “more than 20 million Americans have GERD”. (1) This has important repercussions for our ears. Let me explain.
“When you eat or drink, food and liquid move from your mouth to the esophagus, where a valve, called the lower esophageal sphincter (LES), relaxes to allow the food and liquid to pass into your stomach. The lower esophageal sphincter then squeezes shut to keep stomach contents from backing up (a process known as reflux) into the esophagus.” (1)
As long as this valve stays tightly shut, you don’t have a problem. However, when it relaxes, the contents of your stomach can be forced into your esophagus and cause GERD problems there.
I just ran across an interesting article (1) that details some of the reasons for the LES relaxing. I think you’ll find it enlightening.
A number of drugs are the culprits. When doctors prescribe drugs to treat conditions such as high blood pressure, heart disease, depression and anxiety, the drugs they prescribe can cause GERD where none existed before.
According to Dr. Anil Minocha, drugs that can cause the lower esophageal sphincter valve to relax (and thus result in GERD) include calcium channel blockers, beta blockers, some antidepressants and some anti-anxiety drugs.
Here’s a list of several of the calcium channel blockers: Amlodipine, Diltiazem, Felodipine, Nicardipine, Nifedipine, Nisoldipine and Verapamil. The more common ototoxic side effects of these calcium channel blockers include ataxia, dizziness, tinnitus and vertigo.
Some of the beta-blockers include: Acebutolol, Atenolol, Betaxolol, Bisoprolol, Carteolol, Carvedilol, Labetalol, Metoprolol, Nadolol, Oxprenolol, Pindolol, Propranolol and Timolol. The more common ototoxic side effects of these beta-blockers include dizziness, ear pain, hearing loss, tinnitus and vertigo.
If you take any of the above drugs, you want to be aware that these (and other) drugs actually reduce lower esophageal sphincter (LES) pressure (that is, they relax this muscle located at the top of your stomach). As a result, the contents of your stomach can then back up into your esophagus, eventually resulting in GERD.
Not only are many of the drugs that help cause GERD ototoxic, but the very drugs that doctors prescribe to control GERD are also ototoxic. Thus your ears can get clobbered both coming and going.
You see, doctors often prescribe acid-reducing prescription drugs such as H2 blockers—Ranitidine (Zantac) and Famotidine (Pepcid), or proton pump inhibitors—Esomeprazole (Nexium) and Omeprazole (Prilosec) to try to control GERD.
Ranitidine is ototoxic and can cause dizziness and vertigo, while Famotidine can cause dizziness, tinnitus and vertigo. Esomeprazole—the little purple pill—can cause ataxia, dizziness, ear pain, tinnitus and vertigo, while Omeprazole can cause dizziness, tinnitus and vertigo.
Thus, when you use even more drugs to “cure” the side effects of other drugs, you can end up increasing the risk of damage to your ears (not to mention the rest of your body). Consequently, you always want to be sure the drugs you are taking aren’t causing other side effects.
Incidentally, in addition to the above drugs, certain foods also relax the LES, and thus are also conducive to causing GERD. Consequently, if you are prone to GERD, watch your intake of things like fatty foods, onions and chocolate.
Furthermore, if you are stressed out, get your stress under control BEFORE you get GERD. You see, stress also causes the LES to relax, again paving the way for GERD.
If you already have GERD, you might want to consider these 4 things:
- Get off any drugs that relax the LES.
- Cut out LES-relaxing foods.
- Get your stress under control.
- Take probiotics such as Lactobacillus acidophilus. These “friendly” bacteria reduce the harmful effects of acid in your esophagus. (1) You can naturally acquire Lactobacillus when you eat yogurt or kefir containing active (live) cultures, or you can purchase Lactobacillus tablets at your health food store.
You don’t have to let ototoxic drugs inadvertently damage your ears. To learn which drugs are (or can be) ototoxic, see “Ototoxic Drugs Exposed“. This book contains information on the ototoxicity of 763 drugs, 30 herbs and 148 chemicals.
Google ”silent reflux secondary endolymphatic hydrops”
Etiology (cause) of Menieres Syndrome
https://www.dizziness-and-balance.com/disorders/menieres/men_eti.html
1. Intestinal permeability. Di Berardino et al (2017) found that ”An altered intestinal permeability, according to the two assays, was found only in symptomatic MD patients”. They studied 26 patients, and 20 controls. This may relate to another study suggesting that mycostatin (which is not absorbed from the gut) improves Meniere’s. This is a pretty far fetched idea.
- GERD (gastroesophageal reflux). Some patients with fluctuating hearing get worse at night, and have reflux. It seems reasonable to suppose that stomach acid or enzymes could be getting into their middle ear. Very little has been written about this idea, although it is clear that reflux can get into the ears of children. We think that this is true in a few patients, and that this mechanism has been neglected.
- Venous drainage. Ciccone et al (2018) reported that in patients with Meniere’s disease as well as suden hearing loss had lower velocity of venous cerebral veins, including the internal jugular and vertebral veins. We think this is interesting and more research is needed.
 Fig. 1a: Normal membranous labyrinth 1b. Dilated membranous labyrinth (Endolymphatic Hydrops)
Fig. 1a: Normal membranous labyrinth 1b. Dilated membranous labyrinth (Endolymphatic Hydrops)
https://www.dizziness-and-balance.com/disorders/menieres/men_eti.html
Inflammaging) and Hearing dysfunctions
See also much more (2021-01-15) new texts http://carism.se/notes/inflammaging-in-general-and-ear-nose-throat-in-particular/
Resolution of Inflammation (including Inflammageing) and Age-Related Hearing Loss (ARHL)
https://www.frontiersin.org/articles/10.3389/fncel.2017.00192/full – https://escholarship.org/content/qt45h1k38c/qt45h1k38c_noSplash_5fcccc3f6510d1bfd6388b48ff30fee7.pdf
“Another key contributor to several age-related diseases, including ARHL, is the state of chronic inflammation in the elderly known as ‘‘inflammaging’’ (Capri et al., 2006; Hunt et al.,
2010; Leng et al., 2011; Baylis et al., 2013; Verschuur et al., 2014). Inflammaging is a consequence of immune-senescence, the aging of the immune system (Capri et al., 2006; Hunt et al., 2010).
A potential link with inflammaging may be very important for ARHL, providing new approaches to prevent the development of this condition.
As a matter of fact, ARHL severity has already been linked to some factors associated with inflammation and inflammaging (Gates et al., 1993; Gates and Mills, 2005; Frisina et al., 2006;
Verschuur et al., 2014). For instance, it has been shown that spiral ganglion cell damage can be caused by changes in the immune system (Iwai et al., 2003, 2008), while vascular and
metabolic changes may affect the stria vascularis and, indirectly, cause inflammatory damage (Saitoh et al., 1995; Ohlemiller, 2009; Fetoni et al., 2011). In a clinical trial an association was
found between serum immunoglobulin G and hearing loss in individuals over 60 years of age (Lasisi et al., 2011). Thus, there is a high probability that inflammation and inflammaging could play a role in ARHL.”
Tinnitus, hearing loss and inflammatory processes in an older Portuguese population – https://www.tandfonline.com/doi/abs/10.1080/14992027.2019.1698775?needAccess=true&journalCode=iija20
“Conclusions: The results of our study showing fluctuations in inflammatory markers along the hearing loss process, reinforce the idea that inflammatory mechanisms are involved in hearing loss pathogenesis but also in tinnitus. IL10 levels appear significantly altered in tinnitus but not in hearing loss.”
Chronic Inflammation – Inflammaging – in the Ageing Cochlea: A Novel Target for Future Presbycusis Therapy https://www.researchgate.net/publication/320354252_Chronic_Inflammation_-_Inflammaging_-_in_the_Ageing_Cochlea_A_Novel_Target_for_Future_Presbycusis_Therapy
“Chronic, low-grade inflammation, or inflammaging, is a crucial contributor to various age-related pathologies and natural processes in aging tissue, including the nervous system. Over the past two decades, much effort has been done to understand the mechanisms of inflammaging in disease models such as type II diabetes, cardiovascular disease, Alzheimer’s disease, Parkinson’s disease, and others. However, despite being the most prevalent neurodegenerative disorder, the number one communication disorder, and one of the top three chronic medical conditions of our aged population; little research has been conducted on the potential role of inflammation in age-related hearing loss (ARHL). Recently, it has been suggested that there is an inflammatory presence in the cochlea, perhaps involving diffusion processes of the blood-brain barrier as it relates to the inner ear. Recent research has found correlations between hearing loss and markers such as C-reactive protein, IL-6, and TNF-α indicating inflammatory status in human case-cohort studies. However, there have been very few reports of in vivo research investigating the role of chronic inflammation’s in hearing loss in the aging cochlea. Future research directed at better understanding the mechanisms of inflammation in the cochlea as well as the natural changes acquired with aging may provide a better understanding of how this process can accelerate presbycusis. Animal model experimentation and pre-clinical studies designed to recognize and characterize cochlear inflammatory mechanisms may suggest novel treatment strategies for preventing or treating ARHL. In this review, we seek to summarize key research in chronic inflammation, discuss its implications for possible roles in ARHL, and finally suggest directions for future investigations.”
Herpes zoster and Tinnitus
Ramsay Hunt Syndrome –
“Ramsay Hunt syndrome, also known as herpes zoster oticus or geniculate zoster, is a rare condition that manifests as a complication of the Varicella zoster virus (VZV) that arises in the geniculate ganglion of cranial nerve CVII.[1] Early stages of the VZV infection cause fever and diffuse vesicular rash, a condition that is commonly referred to as chickenpox. After the initial infection, the virus will often remain dormant within various ganglion in the body. The zoster infection is caused by a reactivation of the virus. This can produce linear vesicular rashes along the nerve’s distribution, typically involving a single dermatome. The distribution and associated symptoms depend on the nerve involved, and there are many different syndromes associated with this virus. Less than 1% of the cases of zoster involve the facial nerve and result in Ramsay Hunt syndrome.[2] The syndrome is characterized by a classic triad of ipsilateral facial paralysis, otalgia, and vesicles in the auditory canal.[3] Additional symptoms include changes in taste along the anterior two-thirds of the tongue, dry eye, hearing loss, tinnitus, and/or vertigo can be seen with the involvement of the vestibulocochlear nerve. Vesicles often develop after the onset of neurologic symptoms. Vesicles typically appear near the ear but can be seen along the affected side of the face, hard palate, and tongue”.
BvS-> As I suffered from very severe Herpes Zoster (HZ) which was influencing in a complex manner (including eyes clearly) and this has turned up (after this main very hard disease period, , e.g. had problems to move and weeks before I could walk normally – to late diagnose identified for any Zovirax) symptoms possible related to HZ. As HZ last 15 years has been associated with Tinnitus, I also insert some information at this website!
Ramsay Hunt syndrome
https://jnnp.bmj.com/content/71/2/149
” The strict definition of the Ramsay Hunt syndrome is peripheral facial nerve palsy accompanied by an erythematous vesicular rash on the ear (zoster oticus) or in the mouth. J Ramsay Hunt, who described various clinical presentations of facial paralysis and rash, also recognised other frequent symptoms and signs such as tinnitus, hearing loss, nausea, vomiting, vertigo, and nystagmus.”
See also; https://rarediseases.org/rare-diseases/ramsay-hunt-syndrome/ – https://www.sciencedirect.com/science/article/pii/B9780721603346500509 – https://www.sciencedirect.com/topics/medicine-and-dentistry/herpes-zoster-oticus –
https://journals.lww.com/md-journal/fulltext/2016/11150/Characteristics_of_hearing_loss_in_patients_with.60.aspx –
How is endoymfatic hydrops produced, what influence it and what can we do clinically?
(see also below ”Weather, Tinitus and especially Endolymfatic Hydrops”)
Above an overview as well as a picture showing how Endolymphatic Hydrops look like compared with normal. See also the text which is an excellent overview …
https://www.menieres.org.uk/information-and-support/symptoms-and-conditions/endolymphatic-hydrops
In brief; “Endolymphatic hydrops is a disorder of the vestibular system in the inner ear. It is thought to stem from abnormal fluctuations in the fluid called endolymph which fills the hearing and balance structures of the inner ear. This condition results in a distended endolymphatic space and is referred to as endolymphatic hydrops. Endolymphatic hydrops is referred to as primary or secondary. Primary idiopathic endolymphatic hydrops, known as Ménière’s disease, occurs for no known reason. Secondary endolymphatic hydrops
Secondary endolymphatic hydrops occurs in response to an event, such as head trauma, allergy or an underlying condition, such as an autoimmune disorder. The symptoms of endolymphatic hydrops include tinnitus, dizziness, fluctuating hearing loss, imbalance and a feeling of fullness/pressure in the ear. Ménière’s disease and endolymphatic hydrops are often used synonymously. Ménière’s disease is idiopathic, meaning that if the cause of vertigo is known the diagnosis cannot be Ménière’s disease. People diagnosed with Ménière’s disease are thought to have endolymphatic hydrops; however not all people diagnosed with endolymphatic hydrops have Ménière’s disease”
Examination: “Reappraisal of the glycerol test in patients with suspected Menière’s disease” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4392460/ “Recent advances in magnetic resonance imaging make it possible to visualize the presumed pathophysiologic correlate of Menière’s disease: endolymphatic hydrops. As traditional diagnostic tests can provide only indirect evidence, they are hardly competitive in this respect and need to be rethought. This is done here for the glycerol test.
Surgery: Myringotomy and Tympanostomy Tube Insertion – information at https://en.wikipedia.org/wiki/Myringotomy or https://www.unicare.com/dam/medpolicies/unicare/active/guidelines/gl_pw_c178412.html
OVERVIEW
Endolymphatic Hydrops
https://www.californiaearinstitute.com/ear-disorders-endolymphatic-hydrops-ear-institute-bay-area.php
- What is endolymphatic hydrops?
Endolymphatic hydrops is a disorder of the vestibular system, which is part of the inner ear. Endolymphatic hydrops consists of abnormal fluctuations in the endolymph fluid, which fills the hearing and balance structures of the inner ear. These fluctuations cause an increase in pressure in the endolymphatic system of the inner ear. Endolymph fluid, which is regulated by the endolymph sac, flows through the inner ear and is critical to hearing. In addition to water, endolymph fluid contains salts such as sodium, potassium, chloride and other electrolytes. If the inner ear is damaged by disease or injury, the volume and composition of the endolymph fluid can also change, causing the symptoms of endolymphatic hydrops.
2. Symptoms of endolymphatic hydrops?
The symptoms of endolymphatic hydrops include the feeling of pressure or fullness in the ears, hearing loss, tinnitus, (ringing in the ears), hearing loss, and balance problems. Individuals who have Meniere’s disease have a very severe form of endolymphatic hydrops, but individuals with endolymphatic hydrops do not always progress to Meniere’s disease.
- What are the causes of endolymphatic hydrops?
Endolymphatic hydrops may occur as a result of trauma such as a blow to the head, infection, degeneration of the inner ear, allergies, dehydration and loss of electrolytes or in rare circumstances a benign tumor. In many cases, it is not clear what causes the disorder. Meniere’s attacks occur when there is an increase in endolymphatic pressure in the inner ear, causing a leak in the membrane separating the perilymph (potassium poor extracellular fluid) and the endolymph (potassium rich intracellular fluid). The mix of these two fluids surrounding the vestibular nerve receptors creates an electrical blockade and a loss of function. The sudden change in the rate of the vestibular nerve firing creates acute vestibular imbalance otherwise known as vertigo.
- What is the treatment for endolymphatic hydrops?
 A specialized interdisciplinary team of professionals is necessary to treat all of the issues associated with Endolymphatic hydrops. This group of individuals should include an Otologist or Otolaryngologist, and an audiologist, and possibly a vestibular rehabilitation expert.
A specialized interdisciplinary team of professionals is necessary to treat all of the issues associated with Endolymphatic hydrops. This group of individuals should include an Otologist or Otolaryngologist, and an audiologist, and possibly a vestibular rehabilitation expert.
Over our forty-year history, CEI neurotologists have developed and refined a three level treatment strategy for patients with Endolymphatic hydrops. The three levels begin with dietary and lifestyle modifications, then medication, and in some cases, a physical therapy and exercise program. In those patients who fail to respond to first measures, more aggressive treatment is needed and may include surgery to stop the attacks of vertigo. Over 90 % of CEI patients successfully have their vertigo controlled with this strategy.
The California Ear Institute is a leading global center for otological, otolaryngological and audiological treatment. Dr. Joseph Roberson, a board certified neurotologist, has performed thousands of successful hearing related surgeries, including many on patients whose hearing impairment is the result of Endolymphatic hydrops.
What are the consequences of avoiding treatment?
Patients must seek medical treatment for any change in hearing or balance regardless of whether or not Endolymphatic hydrops is suspected to be the source of the hearing loss. Evaluation for beneficial drug treatment or surgery cannot be established without a comprehensive medical examination and associated testing. Avoiding medical evaluation for Endolymphatic hydrops or any other hearing or balance impairment related condition is not recommended, and can lead to permanent hearing loss.
Endolymfatic Hydrops and Eustachian dysfunctions
Ménière’s: why its diagnosis calls for more careful evaluation – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5697545/
“DIFFICULTIES IN DIAGNOSING MÉNIÈRE’S – The triad of vertigo, tinnitus, and deafness is a familiar presentation in a GP surgery, but diagnosis and treatment remain a challenge. ‘Difficulty with everything in general practice is spotting the unusual from the commonplace, and continuity of care is really important’, says Dr Henrietta Hughes, GP and National Guardian for the NHS. ‘If a patient comes back to see several different people, they might all try something to fix the immediate problem rather than seeing the whole picture’ (personal communication, January 2017).
There is no definitive test for Ménière’s syndrome and it is not at all uncommon for people to be misdiagnosed. The classic symptoms are fluctuating hearing loss, low-pitch tinnitus, fullness in the ear, and episodic spinning vertigo that lasts at least 20 minutes, but typically 2–3 hours. (The whole attack should be over in less than 24 hours.) A number of recent studies examining the experiences of dizzy patients1–3 have indicated that doctors frequently diagnose it when they see any vertigo they don’t understand, and there are patients diagnosed with Ménière’s syndrome who simply never get evaluated for anything else. Taking the history of a dizzy patient is essential to differentiate the possible aetiologies of vertigo, and a systematic approach must be used. The mnemonic ‘SO STONED’4 has been proposed, summarising the key factors that allow a first approximation of diagnosis identification: Symptoms, Often (frequency), Since, Trigger, Otology, Neurology, Evolution, and Duration. The most common vestibular diseases have different fingerprints when all these factors are examined”.
“MÉNIÈRE’S AS SECONDARY DISORDER – (BvS see also Secondary Endolymfatic Hydrops, SHE, which is obviously the same – see above headings!). When considering Ménière’s, it is important to distinguish between Ménière’s disease, when the cause cannot be identified (idiopathic in other words), and Ménière’s syndrome, when it is secondary to another disorder. There is a long list of possible causes, including hypothyroidism, tumours (most notably acoustic neuromas),5 infections, metabolic or immune disorders, perilymphatic fistula, genetic mutations,6 superior semicircular canal dehiscence syndrome (SCDS), and many more. Treating the underlying cause often resolves the Ménière’s syndrome with much greater success than the non-specific treatments employed for Ménière’s disease. A drug that works for one person does not necessarily work for another because the underlying reasons for the syndrome are so varied and the complex pharmacokinetics of the inner ear make drug delivery to it a tricky business”.
Refractory Eustachian Tube Dysfunction: Are the Symptoms Related to Endolymphatic Hydrops – https://clinicaltrials.gov/ct2/show/NCT01661777
“Eustachian tube dysfunction is one of the most common problems encountered in general otolaryngology clinical practice. Symptoms of ear pressure, decreased hearing, ear pain, ear popping, and frequent ear infections are often blamed on the inability of the Eustachian tube to equalize air pressure across the ear drum. If the Eustachian tube is occluded, the middle ear space becomes a closed chamber in which normal gas exchange cannot occur. Treatment of Eustachian dysfunction has traditionally focused on a two tier system. First, patients are most often placed on a nasal steroid and an antihistamine. This medication regimen leads to decreased nasal inflammation, mucosal swelling, and treats nasal allergy. In many patients, this treatment improves symptoms completely or reduces them to a tolerable level. If the patient’s symptoms are not improved, the next step in management is to create a surgical tract to the middle ear via a myringotomy (a hole across the ear drum) and placing a pressure equalization tube across the tympanic membrane. This bypasses any anatomical obstruction in the Eustachian tube and allows the middle ear pressure to equalize with the atmospheric pressure across the tympanic membrane. Unfortunately, despite this, there are patients with refractory symptoms, often ear pressure and subjectively decreased hearing. These symptoms are also frequently associated with inner ear disease, specifically endolymphatic hydrops. Endolymphatic hydrops is felt to be related to over production of endolymphatic fluid, the fluid within the inner ear. Thus, we propose that patient’s will refractory Eustachian tube dysfunction are experiencing an inner ear phenomenon, and that they would benefit from treatment similar to how endolymphatic hydrops (or over production of endolymphatic fluid) is managed. The mainstays of management of endolymphatic hydrops are a low sodium diet and diuretic treatment (hydrochlorothiazide/triamterene). Both of these treatments aim to reduce endolymph production.”
Endolymphatic hydrops mimicking obstructive Eustachian tube dysfunction: preliminary experience and literature revie – https://www.researchgate.net/publication/342422718_Endolymphatic_hydrops_mimicking_obstructive_Eustachian_tube_dysfunction_preliminary_experience_and_literature_review
“PurposeAural fullness is a common symptom of middle ear diseases, most importantly Eustachian tube dysfunction (ETD). Yet, aural fullness may also be caused by inner ear disorders, such as hydropic ear diseases. Here, we report our experience with endolymphatic hydrops (EH) mimicking ETD. Furthermore, we review the literature related to (i) EH as a differential diagnosis of symptoms suggesting ETD and (ii) the pathophysiology and treatment of aural fullness due to inner ear disorders.Methods We retrospectively included adult patients with aural fullness as chief complaint and radiographically diagnosed EH. Hearing and Eustachian tube function were assessed using audiometry, tympanometry, and tubomanometry. Primarily suspected ETD was treated by balloon dilatation of the Eustachian tube (BDET). The endolymphatic space of the inner ear was imaged using gadolinium-enhanced MRI (Gd-MRI) including a 3D-real inversion-recovery sequence after intravenous gadolinium administration.ResultsWe report three affected ears of two patients (two females, age 42 and age 51) with aural fullness as chief complaint. Audiometry of main speech frequencies was normal in all affected ears. In one ear, there was a type A tympanogram and in two ears, there was a type B tympanogram. In both patients, medical treatment for ETD and BDET were unsuccessful. Gd-MRI of the inner ears revealed cochlear EH in 3/3 ears affected by aural fullness, but not in the unaffected ear.ConclusionEH may underlay cases with aural fullness and could in these cases explain unsuccessful treatment for ETD. As ETD is often treated by invasive procedures, distinguishing ETD from EH as the underlying cause of aural fullness is important. Our findings raise the question whether Gd-MRI to rule out EH is indicated in patients with unexplained aural fullness, in particular after unsuccessful interventional treatment for ETD”.
Endolymph Drainage System in Meniere’s Disease
A 3-Dimensional Analysis of the Endolymph Drainage System in Meniere’s Disease Short running title: 3D analysis of endolymph drainage system – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5253118/
“…. One hypothesis regarding why smaller endolymphatic compartments could cause symptoms is based on the principle of “functional reserve.” Smaller vestibular aqueducts and smaller endolymphatic ducts and sacs (smaller because of developmental, environmental, infectious, or even genetic issues) could be complicating factors in the advent of abnormalities in endolymph homeostasis” … “conclusion: Our findings demonstrate that temporal bones of patients with Meniere’s disease had lower volume of the vestibular aqueduct, endolymphatic duct, and intratemporal portion of the endolymphatic sac, and smaller external aperture of the vestibular aqueduct as compared specimens with endolymphatic hydrops without vestibular symptoms and with nondiseased specimens. The open status of the Bast’s valve in the Meniere’s group could be secondary to higher retrograde endolymph pressures caused by smaller drainage systems. These anatomic differences may relate to the cause of clinical symptoms in Meniere’s disease”.
.. “Abnormal amount of fluid in the inner ears” .. is one of the factors that can cause hydrops. Things that might affect the fluid include: Improper fluid drainage, Allergies, Viruses, Genetics, Migraine headaches, Head trauma and Abnormal immune response“ http://www.ucihealth.org/medical-services/ear-nose-throat-ent/hearing-ear-disorders/menieres-disease
… “ .. fluctuation in inner ear fluid can cause the symptoms of hydrops, including pressure or fullness of the affected ear, tinnitus, hearing loss, and imbalance or dizziness. Treatment of this condition is geared towards stabilizing the body fluid levels so that fluctuations in the endolymph volume can be avoided.” https://www.dallasear.com/conditions-menieres.html
What Causes the Accumulation of Fluid in the Ear? https://www.verywellhealth.com/diagnosis-and-treatment-for-fluid-in-the-ear-1192211 “…The auditory tube allows fluid to drain from the ear into the back of the throat. If the auditory tube becomes clogged, fluid will become trapped in the middle ear space. …. In addition to ear infections, the common cold and allergies can often lead to fluid in the ear if inflammation or mucous prevent the auditory tube from draining … All cases of fluid in the ear are caused by some form of auditory tube dysfunction which prevents your eustachian tube from adequately draining” … The auditory tube, sometimes called the eustachian tube, is a tiny channel that runs from the middle ear to the back of the throat (nasopharynx). The auditory tube has several important functions:
It opens and closes in response to changes in ambient air pressure in order to equalize pressure in the middle ear.
It may close in response to loud noises to protect delicate ear structures.
It clears mucus from the middle ear, allowing it to drain into the back of the throat.
The auditory tube in children runs at a more horizontal angle than in adults. With age, the tube enlarges and gradually becomes more vertical to facilitate better drainage. This explains why children are more prone to auditory tube problems.
While the auditory tube is normally closed, it does open periodically such as when we swallow, yawn, or sneeze. This explains why we often need to swallow in order to ”pop” our ears when driving up a mountain or taking off in an airplane. When you swallow, your auditory tube opens and equalizes the pressure automatically … If mucus is not properly cleared, it can lead to middle ear infections (otitis media), fluid in the ear (serous otitis media), or hearing loss caused by changes in the position of the eardrum (middle ear atelectasis). These conditions can result in pain, hearing loss, dizziness, and even ear damage.” https://www.verywellhealth.com/about-auditory-eusctachian-tube-dysfunction-1191872
 When you yawn or swallow, the eustachian tubes open briefly and make the air pressure equal inside and outside the ears (top picture). The eustachian tubes drain fluid from the ears. But if a tube can’t open, fluid can get trapped in the middle ear (bottom picture). This creates pressure that can cause ear pain. https://www.uofmhealth.org/health-library/uf9680
When you yawn or swallow, the eustachian tubes open briefly and make the air pressure equal inside and outside the ears (top picture). The eustachian tubes drain fluid from the ears. But if a tube can’t open, fluid can get trapped in the middle ear (bottom picture). This creates pressure that can cause ear pain. https://www.uofmhealth.org/health-library/uf9680
Eustachian Tube Dysfunction (ETD) “ … The eustachian tubes help regulate ear pressure and drain excess fluid from the middle ear, moving it to the throat to be eliminated. The canals in these tubes are tiny so blockages can happen for many reasons. Blocked eustachian tubes can cause discomfort and hearing problems, and any of these symptoms can be referred to as ETD”.
Causes: ETD covers a broad range of symptoms and has a range of potential causes. Season allergies and illnesses that create inflammation in the area, such as the flu or cold, are common causes of ETD. Sinus infections can also trigger ETD, as a sinus infection causes the eustachian tubes to become inflamed or filled with mucus. More serious infections can cause ETD as well.
Simple changes in altitude or air pressure may also trigger ETD. Driving up a mountain or sitting in a plane can cause ETD, and even just riding the elevator in a tall building may be enough for some people to develop unpleasant symptoms. ”. https://www.medicalnewstoday.com/articles/319602
Interventions for adult Eustachian tube dysfunction: a systematic review https://www.ncbi.nlm.nih.gov/books/NBK262265/ “… Eustachian tube dysfunction (ETD) is the inability of the Eustachian tube to adequately perform these functions. However, the precise function and mechanisms of the Eustachian tube and the underlying causes of dysfunction are complex and not fully understood.1 From a diagnostic perspective, ETD is also poorly defined.
Eustachian tube dysfunction may occur when the mucosal lining of the tube is swollen, or does not open or close properly.2 If the tube is dysfunctional, symptoms such as muffled hearing, pain, tinnitus, reduced hearing, a feeling of fullness in the ear or problems with balance may occur. Long-term ETD has been associated with damage to the middle ear and the eardrum.3 Complications include otitis media with effusion (glue ear), middle ear atelectasis (retraction of the eardrum), and chronic otitis media.1,3 However, the role of the Eustachian tube in the development of other middle ear conditions is not fully understood.1 Middle ear ventilation is increasingly seen as being associated with other mechanisms, such as those relating to gaseous exchange through the middle ear mucosa.4,5 Therefore, it may be that problems with middle ear ventilation (and therefore symptoms and signs previously attributed to ETD) may not all be associated with problems with or dysfunction of the Eustachian tube”.
About Eustachian Tube Dysfunctions
Eustachian Tube Function and Dysfunction
Figure 10–1 Schematic of the eustachian tube valve. (See Color Plate 10-1)
”The eustachian tube is a dynamic conduit that connects the middle ear with the nasopharynx. It contains secretory, ciliary, and dilatory functions. The eustachian tube regulates air pressure within the middle ear and mastoid system, clears material out from the middle ear, and prevents the reflux of material and sound from the nasopharynx into the ear. The tube contains a physiologic valve that is closed in the passive resting position and is dilated open by active muscular exertion. There is no generally accepted definition for eustachian tube dysfunction, but it is commonly taken to imply an inadequate ability to open the tubal valve …
Opening and Closing of the Eustachian Tube: A great deal has been learned about the mechanisms of eustachian tube opening through experimentation with phototubometry, sonotubometry, manometric measurements, contrast radiography, and electrical stimulation of tubal muscles in dogs and monkeys.1,18,28 Contrast radiography in animal models and humans has demonstrated a consistent pattern of opening and closing along the length of the cartilaginous tubal lumen. The osseous eustachian tube remains unchanged and patent throughout the dilatory and closing sequence. The cartilaginous tube is initially closed in the resting position. The dilation begins at the nasopharyngeal orifice and progresses distally toward the bony isthmus. Tubal closure reverses the process progressing from distal to proximal and produces the “pumping action” that has been previously described.” https://entokey.com/eustachian-tube-function-and-dysfunction/
See more below about patulous and when the tube becomes stuck in the open position
The Eustachian Tube pictures
www.ent-surgery.com.au/the-eustachian-tube
http://www.kids-ent.com/newkids800/earframe.html
ETD Treatments include :
https://med.uth.edu/orl/texas-sinus-institute/patient-education/eustachian-tube-dysfunction/
There are several treatment options for ETD ranging from simple to more invasive. In most cases, once the underlying cause of the ETD (cold, allergies, or flu) resolves, ETD symptoms will also improve.
Treatments include:
The patient can “autoinsufflate” – to do this, the patient NYPA pinches his or her nostrils and then exhales with a close mouth. Gentle blowing during this maneuver will also force air into the Eustachian tube and thus “pop” it open
NB “pinches nostrils and then exhales with a close mouth”
Oral decongestants, topical decongestant or oral steroids may be prescribed to decrease the swelling at the Eustachian tube.
Topical nasal steroids (fluticasone, plus many others) and oral antihistamines (loratadine, plus many others) may be used to treat allergies.
Ear tubes (small tubes that are place into the tympanic membrane) directly equalize the pressure and drain the fluid behind the ear drum. This procedure may be performed in the office for adult patients.
Balloon dilation of the Eustachian tube is a relatively new treatment for ETD.
Also a brief information about Eustachian https://www.ent-surgery.com.au/the-eustachian-tube/
More text introduction;
https://www.buckshealthcare.nhs.uk/Downloads/Patient-leaflets-ENT/PET-001%20Patulous%20Eustachian%20Tube%20v2.0%20rvw%2004%202021.pdf
” The Eustachian tube is normally closed in the resting position and prevents air and fluid as well as sound from passing from the back of the nose and throat up into the ear. The Eustachian tube is supposed to open to regulate air pressure inside the middle ear and typically does this during a strong swallow or a yawn.
When patulous, the Eustachian tube becomes stuck in the open position and causes voice and breathing noises from the nose and throat to travel up the tube and be heard loudly in the ear. It can also cause a sensation of pressure changes in the ear with breathing. It is often difficult for doctors and even specialists to make an accurate diagnosis of this condition.
https://www.audiologyonline.com/ask-the-experts/relationship-between-eustachian-tube-dysfunction-144
The human Eustachian tube is of immense importance in regulating the cavity of the middle ear as well in contributing to voice modulation. The tensor tympani muscle, the muscle connecting the tympanic membrane with the upper end of the Eustachian tube, opens the normally-closed isthmus by yawning, swallowing, and less dependably by chewing. In terms of swallowing, the most common form of activation, it is estimated that about every third or fourth swallow causes the tensor tympani to open the isthmus area so that the otherwise air-tight middle ear cavity can equalize air-pressure to that of the external auditory canal (EAC) side of the tympanic membrane. At this point, there are two main tinnitus/Eustachian abnormalities that can occur here:
If the Eustachian tube stays closed, as during inhalant allergy, head cold, or middle ear infection, the oxygen trapped in the middle ear cavity is soon absorbed into the mucosa, creating a vacuum. The ensuring vacuum causes the cavity to fill with mucous. If uninterrupted, it will continue to do so until the pressure can cause tympanic membrane perforation. It is that in-between state that presents varying types of possible objective tinnitus: roaring, buzzing, humming, heartbeat, and in some cases, spasm of the tensor tympani and/or venous hum (when the pressure on vascular structures and surrounding tissues become too great). All of this, of course, can be ascertained through tympanometry, otoscopy, and other diagnostic measures.
If the Eustachian stays open (Patulous) as from physical abnormality, one will likely experience another type of objective tinnitus: described as an ocean roar or hollow effect, like a sea shell. In some cases, other palatal and middle ear structures may be involved, bringing even more complex descriptions of tinnitus.
Treatment varies according to underlying etiology, involving decongestants, antihistamines, antibiotics, surgery, manipulation, etc. Only a physician can determine appropriate treatment. Since we are speaking primarily of objective tinnitus here, we expect the tinnitus to subside with treatment. However, often there are cochlear, vascular, and other overlays that leave some remaining or changed expression of tinnitus. For more definitive information on the various types of tinnitus and middle ear relationships, the reader may go to www.utmb.edu/otoref/Grnds/Tinnitus-030122/Tinnitus-030122.htm.
Dr. Chartrand has served actively in the hearing health field for almost 32 years. His works are available in textbooks, hundreds of papers and articles, and on the Internet. He is Associate Professor of Behavioral Medicine at North Central University, and Director of Research at DigiCare Hearing Research & Rehabilitation.
Predominance of left ear in Meniére’s disease, sudden deafness, inner ear damage, tinnitus and abnormally patent eustachian tube – https://pubmed.ncbi.nlm.nih.gov/8482264/
Unilateral patulous eustachian tube with tinnitus, inner ear damage, vertigo and sudden deafness–collagen injection https://pubmed.ncbi.nlm.nih.gov/3350700/ ”In elderly patients an unilateral sensorineural hearing loss is frequently associated with a relatively more patent eustachian tube on the involved side. A simple method of investigation is observation under the operating microscope during tubal inflation by the patient. In right-handed patients the abnormally patent tube most often lay on the left side. Powerful self inflation in these patients induces acute hearing loss and vertigo. Acute hearing loss is commoner on the left side. The air bone gap is greater at higher frequencies due to mobility of the stapes, loosening of the incudal joints and the tympanic membrane. In contrast the air bone gap is greater at lower frequencies in otosclerosis or malleus head ankylosis. Minor degrees improve after self inflation is prohibited. In most patients with abnormally patent eustachian tubes further therapy is not necessary after the patient has received precise advice. In only about 20% of the cases is the patient disturbed by a feeling of fullness in the ear, autophony and tinnitus. After stabilisation of weight and blood pressure, a septoplasty with correction of the posterior turbinates may reduce the exspiratory resistance. The most drastic treatment is a collagen injection around the tube. Patients with depression should be treated appropriately”.
Patulous eustachian tube: Treatment, causes, and symptoms – https://www.medicalnewstoday.com/articles/patulous-eustachian-tube
An Overview of Patulous Eustachian Tube
https://www.verywellhealth.com/what-is-patulous-eustachian-tube-1191972
”……
Before receiving treatment, you may find that sniffing or lowering your head can cause some temporary relief of autophony. Mild symptoms may not require any treatment.
The most common treatment for a patulous eustachian tube is nasal sprays. Saline is the most common choice in the United States.
While many inner ear conditions can benefit from nasal decongestants or steroids, the practice will likely worsen your symptoms of PET. If this occurs, treatment should be stopped. If steroids are used, the treatment should be gradually tapered under the supervision of a doctor to prevent a rebound of symptoms and withdrawal side effects.
Invasive Treatments
When less invasive methods prove insufficient to resolve symptoms of a patulous eustachian tube, surgical treatments may be more effective.
Unfortunately, there is not enough evidence to predict which patients will respond positively to the surgical placement of ear tubes. However, ear tube placement is a fairly simple procedure with few side effects and the synthetic tubes can be removed if they do not provide relief for you.
Another less-invasive procedure is referred to as mass loading in which a pressure-sensitive clay-like adhesive called Blu Tack is applied to the eardrum.6 Anesthesia is not required, and the procedure is generally well-tolerated. This is thought to be helpful by reducing the sensation of echo in your inner ear by thickening your eardrum, which reduces its reaction to low-frequency sounds.
Other more invasive therapies that are being studied, and are not available in all areas, include:
- Injecting the eustachian tube with Teflon, silicone, cartilage, or other filling agents
- Surgical placement of cartilage inside the eustachian tube
- Cauterizing the eustachian tube
- Manipulation of the muscles around the eustachian tube
Inserting a catheter inside the eustachian tube, injecting the eustachian tube, or musculature manipulation all allow for a narrowing of the eustachian tube. While this does not return the normal function of the tube, it reduces the amount of airflow into the middle ear, which helps to reduce the symptoms of autophony.
Surgically placing cartilage inside the eustachian tube has a similar purpose to catheter placement and is used only if the catheter has failed.
If all else fails, the otolaryngologist may recommend the complete closure of the eustachian tube. This procedure alone is insufficient to help manage symptoms as you lose the ability to regulate pressure in the middle ear. For this reason, your physician will need permanent ear tubes to help maintain equilibrium. It is an impactful surgery and one that is only used as a last resort
Understanding Superior Semicircular Canal Dehiscence
https://www.verywellhealth.com/superior-semicircular-canal-dehiscence-4098075
Semicircular Canal Dehiscence (SSCD), also called Superior Canal Dehiscence Syndrome (SCDS), is a condition caused by a hole or opening in the bone overlying the superior semicircular canal. The compromised bone allows endolymph in the superior semicircular canal to move in response to sound or pressure stimuli.
Modified Muncie Technique: Osteopathic Manipulation for Eustachian Tube Dysfunction and Illustrative Report of Case https://jaoa.org/article.aspx?articleid=2093698
”In eustachian tube dysfunction, the eustachian tube fails to open sufficiently, resulting in a difference between the air pressure inside and outside the middle ear. This condition can cause pain and hearing loss and may lead to barotitis media, otitis media, tinnitus, and vertigo. Although several treatment options are available, from antibiotics to surgery, little documentation of osteopathic manipulative techniques exists. The current report discusses various treatment options, including the modified Muncie technique—a type of myofascial release administered inside the patient’s mouth—for patients with eustachian tube dysfunction and its symptoms. An illustrative case of a 37-year-old woman who complained of intermittent vertigo and who was treated with this technique is included.”
Eustachian Tube Dysfunction ETD Exercises and Massage Techniques for Ear Fullness https://www.youtube.com/watch?v=1-SZ1r1dnho
Q&A ETD – Eustachian Tube Dysfunction – Other remedies to try https://www.youtube.com/watch?v=Gp0toF7n_wA https://www.youtube.com/watch?v=-Ec6mcKZI0o
Eustachian Tube Dysfunction https://www.youtube.com/watch?v=-Ec6mcKZI0o
EarPopper https://www.earpopper.co.uk/about/
The EarPopper is a clinical device, proven to help restore hearing to normal limits in people suffering from persistent Glue Ear (Otitis Media with Effusion).
”The EarPopper is a device designed to relieve the symptoms of conditions associated with the Eustachian Tube. Based on the Politzer manoeuvre, the EarPopper delivers a safe constant flow of air. When you swallow, the air will pass through the Eustachian Tube helping to ventilate the middle ear.
By using the EarPopper you will be able to relieve the symptoms of negative ear pressure and allow fluids in the middle ear to drain.”
Treatments for Eustachian Tube Dysfunction – https://stanfordhealthcare.org/medical-conditions/ear-nose-and-throat/eustachian-tube-dysfunction/treatments.html
“Eustachian tube dysfunction: Treating allergies and nasal decongestion. Identifying and treating nasal allergies may help to reduce the swelling in the lining of the eustachian tube. There are a number of different ways we can treat allergies, and we will discuss the options with you:
- Identifying the particular allergen you are sensitive to and eliminating it from the environment
- Giving allergy shots, though it may take a long time to notice beneficial effects
- Giving intranasal steroids to reduce inflammation of the mucosal lining of the nose. We usually recommend a two-week trial to see if the medication is helpful.
- Prescribing decongestants, which constrict blood vessels and help open the eustachian tube by reducing swelling of the lining of the nose. These medications work immediately and can be taken as needed. Keep in mind that:
- Oral medications work for about four hours and should not be used around bedtime because they may make it difficult to get to sleep.
- Nasal spray preparations work well and directly decongest the nose; however, because the body rapidly gets used to the medication, they should only be used for up to three days in a row.
- Antihistamines work to reduce the body’s inflammatory response to allergens. These medications may be helpful for some patients and can be taken as needed.
Self-inflation of the ears to treat eustachian tube dysfunction
You may be able to improve your symptoms pinching your nose closed and “popping” your ear. This helps by forcibly air through the eustachian tube into the middle ear. You can also achieve the same effect by blowing up balloons. The pressure required to expand a balloon is usually enough to push air up the eustachian tube.
This is a very useful maneuver and may be repeated as often as necessary, whenever a sense of pressure or fullness in the ear develops. Do not perform this when you have a cold or any nasal discharge because it may drive infected mucous into the middle ear and cause an ear infection.
Surgical treatment for eustachian tube dysfunction
The primary goal of surgical treatment is to bypass the eustachian tube in order to ventilate the middle ear. Surgery can restore hearing, relieve pressure sensation in the ear and reduce the tendency for middle ear infections.
Types of surgery include:
Myringotomy – We make a tiny incision in the eardrum and suction out any fluid in the middle ear. In adults, the incision often stays open long enough to allow the swelling in the Eustachian tube lining to resolve. After the eardrum heals (usually within one to three days), fluid in the middle ear fluid may begin to re-accumulate if the Eustachian tube lining has not recovered.
Pressure equalization tubes – During this procedure we will:
- Make an incision in the eardrum and suction out any middle ear fluid.
- Insert a tiny hollow tube made of plastic or metal into the eardrum
Over time, the tube is pushed out as the eardrum heals. A pressure equalization tube usually provides middle ear ventilation for six to 12 months. Often, the eustachian tube will have recovered by this time, and we will not need to replace the tubes. If you have a more chronic condition, however, we can use longer lasting tubes. In adults, the procedure takes about five minutes and can be performed in the office using a topical anesthetic. In children, we will use a light general anesthetic.
Caring for pressure equalization tubes
It is important to keep water out of your ears when you have pressure equalization tubes. This means:
- Using earplugs or a cotton ball smothered in petroleum jelly while bathing
- Wearing custom earplugs fit to your ear when going swimming
Water that gets into the ear canal can carry bacteria through the tube into the middle ear space and cause an ear infection. This is called a purulent drainage (white, green or yellow pus) from the ear. We treat this type of ear infection with antibiotic eardrops.
The other risk of either a myringotomy or a pressure equalization tube is that the incision may not heal. This may eventually require surgery (tympanoplasty) to patch the hole”.
Balloon dilation for eustachian tube dysfunction: systematic review
https://www.cambridge.org/core/journals/journal-of-laryngology-and-otology/article/balloon-dilation-for-eustachian-tube-dysfunction-systematic-review/04971D25FC698B133C15090056674865/core-reader
”Background: Eustachian tube dysfunction is a disorder for which there are limited medical and surgical treatments. Recently, eustachian tube balloon dilation has been proposed as a potential solution.
Method: A systematic literature review was performed. Abstracts were selected for relevance, and pooled data analysis and qualitative analysis was conducted.
Results: Nine prospective studies, describing 713 eustachian tube balloon dilations in 474 patients (aged 18–86 years), were identified. Follow-up duration ranged from 1.5 to 18 months. Ability to perform a Valsalva manoeuvre improved from 20 to 177 out of 245 ears following eustachian tube balloon dilation and, where data were reported in terms of patient numbers, from 15 to 189 out of 210 patients. Tympanograms were classified as type A in 7 out of 141 ears pre-operatively and in 86 out of 141 ears post-operatively.
Conclusion: Prospective case series can confirm the safety of eustachian tube balloon dilation. As a potential solution for chronic eustachian tube dysfunction, further investigations are warranted to establish a higher level of evidence of efficacy.
Balloon dilation of the Eustachian tube: clinical experience in the management of 126 children – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5782429/
Bielefeld Balloon Catheter http://saomaimed.vn/product/bielefeld-balloon-catheter/

https://www.kebomed.se/produkter/bielefeld-ballong-kateter-361/
Patulous Eustachian Tube Management of Autophony – https://medicine.uiowa.edu/iowaprotocols/patulous-eustachian-tube-management-symptom-autophony
Very much text and Pictures, here especially see “5” below “….
4. Myringotomy with or without placement of tympanostomy tube (Luxford 1982)
Reported as helpful in 50% of cases
Most effective in relieving the sensation of TM moving during breathing
- Mass loading of the eardrum was performed with Blu Tack, a clay-like, nontoxic substance (Bartlett 2010).
Placement of material on the tympanic membrane was useful for short periods providing relief
6. Botulinum toxin A (Botox) injection to peritubal muscles (tensor and levator veli palatini and salpingopharyngeus muscles) (Olthoff 2007)
Single case report of 2.5 units of Botulinum toxin A (Allergan) with symptom relief for 9 months”
Also see;
Youtube info https://www.youtube.com/watch?v=28oT4aFZmNc&feature=share
Eustachian Tube Dysfunction ETD Exercises and Massage Techniques for Ear Fullness
Eustachian Tube Dysfunction and Tinnitus
Tinnitus & Eustachian Tube Dysfunction https://www.laents.com/conditions/tinnitus/
“There are a variety of treatment options available for tinnitus. Some include sound therapy, where specific sounds are played to counteract the ringing. In other cases, tinnitus can be improved with the use of a hearing aid. When it is caused by a medical condition or medication, controlling that medical condition or changing your prescription medication could reduce or eliminate tinnitus. When caused by eustachian tube dysfunction, some allergy medications such as antihistamines or decongestants can manage eustachian tube problems, balance ear pressure, and reduce tinnitus. For some cases, surgery is necessary. The surgery involves placing a pressure equalization tube (PET) in the eardrum, taking the place of the malfunctioning eustachian tube, equalizing inner ear pressure.”
“Dr. Shervin Aminpour is highly regarded as an ear, nose, throat, and allergy doctor. He is an authority in the field and is personally dedicated to helping his patients with tinnitus to treat the condition. Tinnitus is a frustrating condition, and serious cases can make daily activities difficult and stressful. Dr. Aminpour is committed to finding solutions for your hearing, and creates a customized treatment plan for every patient, after identifying the underlying cause of the symptoms. Our friendly and compassionate staff will be happy to assist you at either of our Los Angeles area locations. Schedule a consultation with us today for one of the best treatments of tinnitus Los Angeles has to offer”.
Eustachian Tube Dysfunction https://patient.info/ears-nose-throat-mouth/earache-ear-pain/eustachian-tube-dysfunction ….. Much text … then “What causes long-term Eustachian tube dysfunction? For most people who experience ETD, it settles by itself within a couple of weeks. But in some people, it seems to go on for a long time – many months. It is not known why some people are more prone to this happening than others”.
Some common causes of long-term (chronic) ETD:
Chronic sinusitis – up to half of people with chronic ETD.
Persistent rhinitis.
….
In around 1 in 5 people who have long-term ETD, no cause is found. There is no evidence that there is a genetic cause and it doesn’t appear to run in families.
What You Should Know About Eustachian Tube Dysfunction
https://www.healthline.com/health/eustachian-tube-dysfunction#complications
“The most common complication of ETD is the risk for recurring symptoms. Symptoms are more likely to come back if you don’t treat the underlying causes of ETD.
Complications: In severe cases, ETD may also cause:
Chronic otitis media, also known as a middle ear infection.
Otitis media with effusion, often called glue ear. This refers to fluid buildup in the middle ear. It may last for a few weeks, but more severe cases can cause permanent hearing damage.
Eardrum retraction, which is when the eardrum is seemingly sucked back further into the canal.”
More is coming …
Eustachian tube dysfunctions and Sinus problems
Is Chronic Rhinosinusitis and Status of Pharyngeal End of Eustachian Tube Link-Up: All Smoke No Fire? https://webcache.googleusercontent.com/search?q=cache:9Bw_Foc51PoJ:https://www.ijcmr.com/uploads/7/7/4/6/77464738/_fijcmr_639_may_26.pdf+&cd=13&hl=sv&ct=clnk&gl=se&client=firefox-b-d
ABSTRACT Introduction: Chronic Rhinosinusitis is one of the commonly encountered problems in otorhinolaryngology practice. Aim was to study the effect of Chronic Rhinosinusitis on pharyngeal end of Eustachian tube opening by nasal endoscopy, and to emphasize the need for proper diagnostic endoscopic evaluation in Eustachian tube dysfunction. Material and Methods: Eighty three patients of Chronic Rhinosinusitis, in the age group of 18-65 years, were identified. Eighty three patients were selected as control group having asymptomatic deviated nasal septum and no subjective or objective evidence of chronic rhinosinusitis. The changes at the pharyngeal end of the Eustachian tube were assessed by endoscopy, according to the types of changes, graded from I to V. Results: Evaluation revealed that Chronic Rhinosinusitis causes changes at the pharyngeal end of the Eustachian tube in 81.92% (68/83) cases. Type I (normal Eustachian tube) was seen in 18.08% (15/83). Type II changes were seen in 71% (59/68) cases, type III changes were seen in 13.23% (9/68) cases. In control group normal ET orifice was seen in 74.69%, Type II changes were seen in 18.07% and type III changes in 7.22% cases. Conclusion: Chronic Rhinosinusitis cause changes at the pharyngeal end of Eustachian tube, in the form of congestion, mucosal oedema and blockage of tube. This in turn can lead to middle ear disease. Nasal endoscopy should be done in all the cases of chronic rhinosinusitis, to examine nose, nasopharynx and pharyngeal end of Eustachian tube.
.. When Your Eustachian Tubes Malfunction – https://www.everydayhealth.com/ear-nose-throat/eustachian-tube.aspx
A number of things can go wrong with your eustachian tubes and middle ear, including:
Blockage due to swelling. It is not uncommon for people with sinus pressure to experience middle ear blockage due to congestion of the eustachian tubes. This swelling is most commonly caused by a sinus infection, a cold, or allergies. These conditions can cause the inner ear membranes to swell and block the tubes. A blocked eustachian tube cannot circulate air or drain mucus as it should
Mechanical blockage. Sometimes overgrowth of tissues in the back of the nose (such as nasal polyps or the adenoids) can cause ear blockage by obstructing the eustachian tube opening. On rare occasions, a tumor can cause a blockage.
Otitis media (middle ear inflammation or infection). When sinus congestion leads to a blocked eustachian tube, fluid can accumulate in the middle ear and cause it to become inflamed. Similarly, if you have a bacterial sinus infection that spreads into your eustachian tubes, it can cause a middle ear infection, which leads to swelling and more fluid buildup. Otitis media is associated with ear pain and pressure.
Ruptured eardrum. If too much fluid builds up in your inner ear, it could tear your eardrum.
Middle Ear and Sinus Problems https://www.skybrary.aero/index.php/Middle_Ear_and_Sinus_Problems
“Causes of Blockage to the Middle Ear & Sinuses:
Apart from physiological reasons, the anatomic causes of blocked Eustachian tubes and ostia are practically identical and often the two events will occur together.
Most commonly, these causes are both bacterial and viral infections such as colds and flu; however, blockages can also occur as a reaction to allergies and various diseases. Because, in both the middle ear and the sinuses, a blockage means that mucous cannot be removed, it is possible for bacteria to grow in this mucous, causing further infection, such as sinusitis, and therefore prolonging the problem.
Secondary Endolymfatic Hydrops (SEH)
Brain and inner-ear fluid homeostasis, cochleovestibular-type tinnitus, and secondary endolymphatic hydrops – https://www.researchgate.net/publication/6652171_Brain_and_inner-ear_fluid_homeostasis_cochleovestibular-type_tinnitus_and_secondary_endolymphatic_hydrops
Secondary endolymphatic hydrops (SEH) has clinically been found to have a significant incidence of occurrence in patients with subjective idiopathic tinnitus (SIT) of a severe disabling type. The diagnosis is made clinically and has been established by integration in a medical audiological tinnitus patient protocol of the clinical history with results of electrodiagnostic cochleovestibular testing that fulfill the diagnostic criteria of inner-ear disease consistent with Ménière’s disease. SEH is hypothesized to be a factor, not an etiology, influencing the clinical course of SIT. Alterations over time (i.e., delay in the homeostatic mechanisms in normnal function of the fluid compartments of the inner-ear perilymph, endolymph, or brain cerebrospinal fluid) result in endolymphatic hydrops and interference in normal function of the inner ear, with resultant inner-ear complaints that can be highlighted by tinnitus rather than by vertigo. The endolymphatic hydrops may be either localized or diffuse within the cochlear or vestibular labyrinth. The etiologies and mechanisms of cochleovestibular-type tinnitus are multiple and are influenced by the SEH. Classically, the tetrad of symptoms–episodic vertigo, fluctuating sensorineural hearing loss, tinnitus, and ear blockage–associated with the histopathological correlate endolymphatic hydrops has been diagnosed as Ménière’s disease. Specifically, key etiological agents that have been identified as playing a role in the clinical course of tinnitus (e.g., noise exposure, stress) may serve as ”triggers” or stressors (or both), resulting in interference in normal biochemical and physiological function of sensorineural structures in the inner ear or in neural structures in the brain. In both conditions, the alterations over time (i.e., delay) in the clinical manifestation of the tetrad of symptoms of inner-ear dysfunction, when highlighted by SIT rather than vertigo, otherwise fulfill the criteria for diagnosing SEH. The chief complaint of SIT, when presenting as one of the tetrad of inner-ear symptoms and otherwise diagnosed as Ménière’s disease, has also been associated clinically with perfusion asymmetries in brain, identified by nuclear medicine brain imaging (single-photon emission computed tomography [SPECT] of brain), and reflects an interference in homeostasis in the blood-brain labyrinth or blood-brain barriers, with a resulting SEH. The medical significance of the SIT in some patients may be a gradual, progressive sensorineural hearing loss. The inclusion of SPECT of brain in SIT patients demonstrates a global approach for improving the accuracy of diagnosing the SIT symptom, for focusing on the contribution of central nervous system dysfunction to the development of SEH, and for understanding and influencing the clinical course of SIT.
Secondary Endolymphatic Hydrops (SEH)
https://vestibular.org/secondary-endolymphatic-hydrops-seh “The treatment of secondary endolymphatic hydrops (SEH) is somewhat different. Since SEH is secondary to (that is, results from) an underlying disorder, the symptoms tend to be present more continuously, rather than occurring in spontaneous attacks. However, they are often less violent, and SEH may cause less damage to hearing and balance than does Ménière’s disease.
Secondary Endolymfatic Hydrops – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5425947/ – “Recent investigation of secondary endolymphatic hydrops has brought attention to traumatic and inflammatory insults as causes for secondary endolymphatic hydrops. Such etiologies, including post-surgical effects of cochlear implantation and endolymphatic sac ablation; otosclerosis and its operative intervention(s); acoustic and mechanical trauma; medications; and systemic inflammatory processes, have been determined as causes of secondary lymphatic hydrops. Histopathological slides for many of the etiologies of secondary endolymphatic hydrops are presented … Diagnosis of other middle and inner ear pathology has also been described. One case report discusses the impact of intracochlear schwannomas resulting in secondary endolymphatic hydrops, resulting in symptoms of unilateral tinnitus, vertigo, imbalance, and aural fullness (34–38) (Figure 5). Ultimately, such patients present with symptoms of disequilibrium and vertigo, which helps to lead to their diagnosis of schwannoma but also endolymphatic hydrops as a result (34) … Secondary endolymphatic hydrops is a disease process associated with episodic vertigo and fluctuating hearing loss. Certainly a greater understanding of the underlying etiologies and histopathology of SEH is essential to the care of patients with this disease process. More recent investigation of this disease process has pointed to traumatic and inflammatory causes; however, further investigation is needed to better understand SEH”
What is secondary endolymphatic hydrops? https://balanceanddizziness.org/disorders/vestibular-disorders/secondary-endolymphatic-hydrops/ “Endolymphatic hydrops (EN-doe-lim-FAT-ick HI-drops) is a build-up of fluid in the inner ear. This can cause vertigo, hearing loss, tinnitus and feelings of ear blockage or fullness. Primary endolymphatic hydrops happens on its own, without an underlying cause. This is a theory for why Ménière’s disease develops. By contrast, “secondary” means that the fluid build-up was caused by another problem, such as an underlying disease or an injury”.
”What causes SEH? The fluid in the inner ear (known as endolymph) helps the cells in the inner ear to function normally. These cells detect sound, pressure changes, and changes in speed or direction. When there is too much fluid, the cells may not work properly, which can cause hearing loss and vertigo. However, not everyone with endolymphatic hydrops has symptoms.
The build-up of fluid in the inner ear can be caused by trauma (injury) or inflammation. SEH can happen weeks, months or even years after the trigger that caused it. If SEH happens long after a disease, it is known as delayed SEH.”
Endopymfatic hydrops in general
“Abstract: Ménière’s syndrome is an idiopathic disorder of the cochlea and labyrinth. It is caused by endolymphatic hydrops and is a relatively frequent, lifelong disorder affecting patients’ quality of life and work performance. This article presents our clinical experience with the medical treatment of this disease. Patients were treated with a blend of drugs according to their condition (stage of illness and presence of associated diseases).” ….
“Ménière’s syndrome is an idiopathic disorder of the cochlea and labyrinth (of unknown etiology, with clinical features that include fluctuant sensorineural hearing loss, tinnitus, and incapacitating episodic vertigo.) . It is caused by endolymphatic hydrops and is a relatively frequent, lifelong disorder affecting patients’ quality of life and work performance” … http://www.tinnitusjournal.com/articles/our-experience-with-the-medical-treatment-of-endolymphatic-hydrops.pdf
Or .. “Causes. Endolymphatic hydrops may occur as a result of trauma such as a blow to the head, infection, degeneration of the inner ear, allergies, dehydration and loss of electrolytes or in extremely rare circumstances a benign tumor such as an endolymphatic sac tumor” https://e)n.wikipedia.org/wiki/Endolymphatic_hydrops
More of interests;
“The pathology of Meniere’s disease (MD) is well established to be endolymphatic hydrops. However, the mechanism underlying deafness and vertigo of MD or idiopathic endolymphatic hydrops is still unknown. In order to evaluate the pathogenesis of deafness and vertigo in MD, it seems to be rational to investigate the interrelationship between hydrops and inner ear disorders using animals with experimentally-induced endolymphatic hydrops. In spite of intense efforts by many researchers, the mechanism of vertiginous attack has been unexplained, because animals with experimental hydrops usually did not show vertiginous attack.
Recently, there are two reports to succeed to evoke vertiginous attack in animals with experimental hydrops. In the present paper were first surveyed past proposals about underlying mechanism of the development of hydrops and inner ear disorders associated with hydrops, and were discussed the pathogenetic mechanism of vertiginous attack in hydrops. In conclusion, abrupt development of hydrops was thought to play a pivotal role in the onset of vertiginous seizure.”
… “The mechanism underlying the development of hydrops induced by obstruction or dysfunction of the endolymphatic sac/duct is still conjectural. There are three mechanisms to be assumed. The earliest concept was a blockage in the longitudinal flow or endolymph from the cochlea to the endolymphatic duct/sac. Other hypotheses involve osmotic transport or water into endolymph resulting from an increase in colloidal cellular debris, or an increase in osmotically active ionsin the endolymph caused by their poor absorption in the endolymphatic duct/sac.
https://www.aurisnasuslarynx.com/article/S0385-8146(19)30155-5/fulltext
Endolymphatic hydrops: pathophysiology and experimental models https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2923478/
It is well-established that endolymphatic hydrops plays a role in Meniere’s disease, even though the precise role is not fully understood and the presence of hydrops in the ear does not always result in symptoms of the disease. It nevertheless follows that a scientific understanding of how hydrops arises, how it affects the function of the ear, and how it can be manipulated or reversed could contribute to the development of effective treatments for the disease. Measurements in animal models in which endolymphatic hydrops has been induced have given numerous insights into the relationships between hydrops and other pathological and electrophysiological changes, and how these changes influence the function of the ear. The prominent role of the endolymphatic sac in endolymph volume regulation, and the cascade of histopathological and electrophysiological changes that are associated with chronic endolymphatic hydrops have now been established. An increasing number of models are now available that allow specific aspects of the interrelationships to be studied. The cyclical nature of Meniere’s symptoms gives hope that treatments can be developed to maintain the ear in a permanent state of remission, possibly by controlling endolymphatic hydrops, thereby avoiding the progressive damage and secondary pathological changes that may also contribute to the patient’s symptoms.
PHARMACOLOGICAL INTERVENTIONS
(se also anpve) GABAa – Benzodiazepine-Chloride Receptor-Targeted Therapy for Tinnitus Control:
https://pdfs.semanticscholar.org/4841/d6dbacde4e19a5f2ff9d6f487961f3d29c83.pdf
“Treatment options were presented to patients prior to RTT and included instrumentation; medication (e .g., pentoxifylline); treatment of factors known to be identified with development or continuation of severe disabling tinnitus (i.e ., fluctuation in aeration of the middle ears bilaterally; secondary endolymphatic hydrops); and control of noise exposure.
More will come
Weather, Tinnitus and especially Endolympatic Hydrops
The Weather and Ménière’s Disease: A Longitudinal Analysis in the UK: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5224697/
”Furthermore, if MD (Ménière’s Disease) is due to endolymphatic hydrops (28,29), then changes in atmospheric pressure may well, in turn, influence endolymphatic pressure via the middle ear. Humidity was also independently associated with tinnitus, hearing loss, and increased odds of attacks”. ”“This study provides the strongest evidence to date that changes in atmospheric pressure and humidity are associated with symptom exacerbation in MD. Improving our understanding of the role of weather and other environmental triggers in Ménière’s may reduce the uncertainty associated with living with this condition, significantly contributing to improved quality of life.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5224697/
“Rat model experiments suggest that there is an atmospheric pressure sensor in the vestibular system of the inner ear (27). This may help to explain the relationship between atmospheric pressure and MD, where individuals have a compromised vestibular system. Furthermore, if MD is due to endolymphatic hydrops (28,29), then changes in atmospheric pressure may well, in turn, influence endolymphatic pressure via the middle ear.”
“Humidity was also independently associated with tinnitus, hearing loss, and increased odds of attacks. More humid air is less dense and absorbs more sound (30), possibly explaining the reduction in hearing on more humid days. Anecdotal evidence indicates a relationship between tinnitus and humidity, but no studies to date have investigated the relationship between humidity and tinnitus severity. More research is needed to investigate potential aetiological mechanisms linking humidity with the symptoms of MD. There was also evidence of an additive effect of humidity and atmospheric pressure on the odds of an attack, with high humidity low pressure days increasing the odds of an attack by approximately 50% when compared with low humidity, high pressure days”.
Atmospheric Pressure and Onset of Episodes of Menière’s Disease – A Repeated Measures Stud.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4838262/ ” .. Menière’s Disease (MD) is defined as the idiopathic syndrome of endolymphatic hydrops, characterized by sudden spells of rotatory vertigo and hearing loss, tinnitus and aural pressure, caused by a distension of the endolymphatic space of the inner ear. With a prevalence of 200 to 500 per 100.000 [1, 2], it is a rather common inner ear disorder and causes a considerable socioeconomic burden due to its chronic and incurable nature.” .. “Conclusion: Change in air pressure was significantly associated with onset of MD episode”s, suggesting a potential triggering mechanism in the inner ear. MD patients may possibly use air pressure changes as an early warning system for vertigo attacks in the future”.
“Although the symptoms associated with Endolymphatic Hydrops do not include vertigo, they can create constant pain in the ear that does not go away, isolation and depression. For musicians and others that rely heavily on the ear, the diagnosis can potentially be career ending.” https://vestibular.org/spotlight/diane-worthey
Meniere Disease (Idiopathic Endolymphatic Hydrops) https://emedicine.medscape.com/article/1159069-overview “Ménière disease is a disorder of the inner ear that is also known as idiopathic endolymphatic hydrops. Endolymphatic hydrops refers to a condition of increased hydraulic pressure within the inner ear endolymphatic system. Excess pressure accumulation in the endolymph can cause a tetrad of symptoms: (1) fluctuating hearing loss, (2) occasional episodic vertigo (usually a spinning sensation, sometimes violent), (3) tinnitus or ringing in the ears (usually low-tone roaring), and (4) aural fullness (eg, pressure, discomfort, fullness sensation in the ears)”.
BvS comments: As I myself suffer very much from changes in air pressure, I assume that this might be an indication of endolymphatic hydrops, which has been excluded by more than one) specialist “do not think so” based only watching “from outside”.
What about (automatic translation) “In the middle ear, a certain amount of suppression occurs all the time when the air in the ear is absorbed by the mucous membranes. The negative pressure is equalized through the eustachian tube when swallowing or yawning. This repeated suppression may act as a ”suction pump” against the inner ear and is perhaps a factor that produces endolymphatic hydrops. By putting a small (about 1 x 5-10 mm) plastic tube through the eardrum, the negative pressure disappears and thus the ”suction pump effect”. There are no controlled scientific studies of the effect, but we have long-standing and proven experience that the effect is perceived as good and that it is simple, painless and harmless. https://www.yrsel.com/ywp/behandling-av-menieres-sjukdom-2/
BvS – Perhaps the intervention can give the answer about if there are hydrops or no? “the effective … harmless”. If no changes = no hydrops.
SEH clinical approaches
Examination: “Reappraisal of the glycerol test in patients with suspected Menière’s disease” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4392460/ “Recent advances in magnetic resonance imaging make it possible to visualize the presumed pathophysiologic correlate of Menière’s disease: endolymphatic hydrops. As traditional diagnostic tests can provide only indirect evidence, they are hardly competitive in this respect and need to be rethought. This is done here for the glycerol test. Conclusion: Owing to their ability to reveal functional aspects without an obvious morphological correlate, traditional test for Menière’s disease could be decisive for defining the stage of the disease. A distinctive feature of the glycerol test is that it is capable of determining, with high accuracy, whether the pathophysiologic condition of the inner ear is partially reversible. Prospectively, this could help to estimate the chances of specific therapies.”
Endolymphatic Hydrops (Meniere’s Disease) Test http://www.aetna.com/cpb/medical/data/500_599/0571.html
Policy:
Aetna considers dehydration testing with glycerol, urea, or other osmotic diuretics to verify the suspicion of endolymphatic hydrops (Meniere’s disease) medically necessary only in members with atypical presentations of this disease.
Aetna considers dehydration testing experimental and investigational for other indications because its effectiveness has not been established.
Aetna considers the following experimental and investigational because their effectiveness for these indications has not been established:
- Endolymphatic sac immunohistochemistry of aquaporin-2, V2R vasopressin receptor, sodium potassium chloride co-transporter 2 (NKCC2), and transient receptor potential cation channel V4 (TRPV4)
- Genetic testing of KCNE1, KCNE3, SIK1, SLC8A1, and SLC26A4 gene mutation for the diagnosis of endolymphatic hydrops (Meniere’s disease)
- Intravenous gadolinium inner ear magnetic resonance imaging for the diagnosis of Meniere’s disease
- Testing for antibodies against inner ear antigens for the diagnosis of Meniere’s disease
- Vestibular evoked myogenic potential (VEMP) for the diagnosis of Meniere disease and monitoring of disease progression
- Video head impulse test
Study of cochlear hydrops analysis masking procedure in patients with Meniere’s disease and otologically normal adults – https://www.researchgate.net/publication/233957267_Study_of_cochlear_hydrops_analysis_masking_procedure_in_patients_with_Meniere’s_disease_and_otologically_normal_adults
Surgery: Myringotomy and Tympanostomy Tube Insertion – information at https://en.wikipedia.org/wiki/Myringotomy or https://www.unicare.com/dam/medpolicies/unicare/active/guidelines/gl_pw_c178412.html
https://cmisurgery.net/ent/4-signs-you-may-need-a-myringotomy-ear-tubes-in-adults/
“A myringotomy is a surgical procedure performed to relieve inner ear pressure. The procedure is quick and involves a small incision into the eardrum. Ear tubes in adults are used to treat frequent ear infections, hearing loss, excess fluid, and inner ear trauma”
MRI and hydrops
MRI Endolymphatic cochlear and vestibular hydrops in two patients with isolated recurrent vertigo. For the first patient ( A ), axial FLAIR sequence after subtraction showed neither CH nor VH. The cochlear endolymphatic compartment was linear ( dotted arrow ) and the saccule ( continuous arrow ) filled less than 50 % of the entire vestibule. https://www.researchgate.net/figure/MRI-Endolymphatic-cochlear-and-vestibular-hydrops-in-two-patients-with-isolated-recurrent_fig2_274261675
Endolymphatic hydrops in both the cochlea and vestibule
 https://www.researchgate.net/publication/325088938_Dietary_Neurotransmitters_A_Narrative_Review_on_Current_Knowledge Endolymphatic hydrops in both the cochlea and vestibule on the right side demonstrated by gadolinium-enhanced MRI. The images were obtained using 3D inversion recovery turbo spin echo with real reconstruction sequence 4 h after intravenous injection of double doses of Gd-DTPA at Shanghai ENT hospital. In the right cochlea, marked hydrops was detected based on the bright semicircular appearance of the scala tympani and vestibuli (arrowhead) (Yang et al., 2018); in the vestibule, obvious endolymphatic hydrops was defined by an endolymph/total lymph ratio > 33% (¼43%) (arrow) (Nakashima et al., 2009). Scale bar ¼ 10.0 mm. L: left; R: right ear.
https://www.researchgate.net/publication/325088938_Dietary_Neurotransmitters_A_Narrative_Review_on_Current_Knowledge Endolymphatic hydrops in both the cochlea and vestibule on the right side demonstrated by gadolinium-enhanced MRI. The images were obtained using 3D inversion recovery turbo spin echo with real reconstruction sequence 4 h after intravenous injection of double doses of Gd-DTPA at Shanghai ENT hospital. In the right cochlea, marked hydrops was detected based on the bright semicircular appearance of the scala tympani and vestibuli (arrowhead) (Yang et al., 2018); in the vestibule, obvious endolymphatic hydrops was defined by an endolymph/total lymph ratio > 33% (¼43%) (arrow) (Nakashima et al., 2009). Scale bar ¼ 10.0 mm. L: left; R: right ear.
Endolymphatic hydrops imaging: Differential diagnosis in patients with Meniere disease symptoms https://www.sciencedirect.com/science/article/pii/S2211568417301511
More links:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6146579/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5425947/
https://www.scielo.br/scielo.php?script=sci_arttext&pid=S1679-45082019000100800
https://www.menieres.org.uk/information-and-support/visiting-ent-diagnosis-and-testing
https://www.jbsr.be/articles/10.5334/jbsr.1627/
https://radiopaedia.org/articles/meniere-disease
https://www.dizziness-and-balance.com/disorders/menieres/mri-hydrops.html
https://www.researchgate.net/profile/Arnaud_Attye/publication/274261675_Recurrent_peripheral_vestibulopathy_Is_MRI_useful_for_the_diagnosis_of_endolymphatic_hydrops_in_clinical_practice/links/55c9c36208aeca747d673a8c.pdf
How is airwax produced?
Earwax is produced by the ear to clean and protect itself. It’s secreted by glands in the skin that line the outer half of your ear canals. The wax and tiny hairs in these passages trap dust and other foreign particles that could damage deeper structures, such as your eardrum https://www.health.qld.gov.au/news-events/news/ear-wax-cerumen-cotton-bud-ear-cleaning
”Earwax, also called cerumen, is made by the body to protect the ears. The ear wax has both lubricating and antibacterial properties. Untreated buildup can lead to hearing loss, irritation, pain in the ear, dizziness, ringing in the ears and other problems. Earwax can be removed in several ways; some of these methods can be done at home”. https://my.clevelandclinic.org/health/diseases/14428-ear-wax-buildup–blockage see also https://www.mayoclinic.org/diseases-conditions/earwax-blockage/symptoms-causes/syc-20353004
Signs and symptoms of earwax blockage may include:
Earache.
Feeling of fullness in the affected ear.
Ringing or noises in the ear (tinnitus)
Decreased hearing in the affected ear.
Dizziness.
Cough.
https://www.mayoclinic.org/diseases-conditions/earwax-blockage/symptoms-causes/syc-20353004
More is coming
Orienting Response, Habituation, Locus Coeruleus and Reticular Activation Systems, RAS
Discussed below is mostly auditory related processes.
Habituation is assumed to specifically refers to RAS decrease (see picture above) to pre-stimuli conditions when the orienting response or Starlet response id processed at the Limbic appraisal level and “diagnosed” “to be ignored”. Furthermore, assumed is that it is external generated sounds e.g. it can be raindrops or heartbeats or sudden scream. But what happens when a permanent discordant damages tinnitus sound exists? Something not expected by evolution? It seems not so we cannot expect support by habituation (see more below).
Distraction can be used of course but still the dysfunction generated sound clusters are still there, which can be understood as signaling “dysfunction to be dealt with” as long as the sound exists – that is, a continuous warning “take action”, but we do not know how to do. But also the permanent dysfunction of the Tinnitus sound clusters per se can be an adding biopsychosocial stress damaging factor.
Is it possible to both find ways to decrease the sound part and the very dysfunction itself, that is what generates the sound?
Masking is one idea and valgus stimulation another. But they may or may not influence the sound part but hardly the dysfunction, given the whole matter is associated with an severe operational conditioning at only behavioral level, PTSD related or not.
Orienting response:
Let us start with the Orienting Response: “The orienting response (OR), also called orienting reflex, is an organism’s immediate response to a change in its environment, when that change is not sudden enough to elicit the startle reflex. … The orienting response is a reaction to novel or significant stimuli”. https://en.wikipedia.org/wiki/Orienting_response ”… Sokolov’s investigation of OR was primarily motivated in understanding habituation. Provided the first introduction of a novel stimulus, defined in Sokolovian terms as any change from the ”currently active neuronal model” (what the individual is currently focused on), results in OR. However, with repeated introduction of the same stimulus, the orienting response will decrease in intensity and eventually cease.[1] When novel stimuli have an associated contextual significance, repeated stimulus will still result in a sequentially decreasing OR, though at a modified rate of decay.[2]
More text coming
Summarizing: Orientation response and habituation are basic evolutionary developed mechanism for organism’s survival. But when the auditory generated signals are not temporary but long-termed or even chronic (hopefully not permanent!) the RAS does not know whether the signal is mediated or produced in auditory systems.
Also, RAS does not interpret signals but Limbic systems does it. But probably too late to order habituation two pre-stimuli level while there is no pre-stimuli but constant uniform stimuli.
A vicious circle grow with overactivity in Locus Coeruleus (LC) and associated neurotransmittors where also e.g. GABA deficit (see above about GAB and Glutamate) probably is a consequence of such in balance.
Relating to “appraisal of stress”, https://www.tandfonline.com/doi/abs/10.1080/02699930600616080 which concerns according to (not only) my definition Limbic systems appraisal (Zajon vs Lazarus “controversy” relevant here), we can regard the above vicious circle as a self-supplying close loop systems – unfortunately – not very easy to rational interventions but conscious planned interference with not-conscious systems can work but where it is not enough with autonomic nervous systems biofeedback, as I myself, as a master of Respiratory Sinus Arrhythmia (RSA) – biofeedback, have learned! This means that LC control and override ANS control requiring more than traditional biofeedback, integrated or not. It also means that we can expect that chronic biopsychosocial stress is more or less “visible” part of the complex symptoms/problems, where PTSD-patient (diagnosed or not) be particularly vulnerable
I see three possible solutions; one is discussed below but the other not while I will first see to that not destructive side-effects can emerge (those are not pharmacological substances).
It is known since approximately 50 years that Clonidine can block LC with severe side-effects. Discovery of the beta-endorphins in the 70-ties can do the same “job” (also manic jogging side effects which can be self-treated given individuals know how to do), now we know not very much more but assume that associated systems are part of the “Beta-endorphin-effect”. I use this as one of the tools in my toolbox in my manual in my dissertation 1986, and have used carefully in clinically when I regarded it is appropriate. The problem is that it requires time and energy and need to be carefully learned how to individually to be tailored. By definition it can be other activities than jogging! More at https://carism.se/project/projekt-carism/carism-tips/
More …. https://www.sciencedaily.com/releases/2018/12/181227102057.htm ”.. But when those neurons received excitatory input to their dendrites, the cholinergic system was able to massively increase their activity”…. ”It’s as if the cholinergic system has given a ’go’ signal,” says Fletcher, enabling the output neurons of the neocortex to powerfully respond. Importantly, this change was selective, and only apparent when excitatory input was being processed in the dendrites of the ’output’ neurons. ”We have known for some time that the dendrites of the output neurons of the neocortex only become active when animals are actively performing a behaviour, and that this activity is correlated with perception and task performance,” says Williams. This new work demonstrates that the cholinergic system is critical to this transition in mice and rats, allowing the output neurons to perform computations in a state-dependent manner. ”We suggest that this switch also occurs in the human neocortex, allowing us to rapidly switch our state of vigilance and attention,” says Williams. ”Our work therefore provides important insight into how the progressive degeneration of the cholinergic system in disease blunts human cognition.”
Neural networks of tinnitus in humans: Elucidating severity and habituation https://www.sciencedirect.com/science/article/abs/pii/S0378595515001987
”.. A possible model of habituation to tinnitus is described, that of the attention system (via the frontal cortex) suppressing the response from the amygdala and the use of alternate nodes of the limbic system such as the insula and the parahippocampal gyrus when mediating emotion”.
Habituation deficit in auditory event-related potentials in tinnitus complainers https://www.sciencedirect.com/science/article/abs/pii/S0378595503001722 ”.. According to Hallam’s habituation theory of tinnitus, most of the suffering caused by tinnitus is due to difficulties in habituation to the perceived tinnitus sound. Thus tinnitus complainers are assumed to display a less pronounced habituation as compared to tinnitus non-complainers. In the present study, an experimental test of this theory was undertaken using event-related potentials (ERPs) as indicators of habituation to exogenously administered tone pips. In 22 patients (10 tinnitus complainers and 12 tinnitus non-complainers) and 10 healthy controls, the habituation of ERPs to series of auditory stimuli across four consecutive trials was studied. Diminuition of the N1 and P2 amplitudes of the ERPs was taken to measure the habituation process across the trials. Tinnitus complainers showed a less distinct habituation of the N1−P2 amplitude difference (vertex potential) compared to tinnitus non-complainers. The results are in accordance with Hallam’s theory and support the notion that patients with a severe tinnitus fail to properly habituate to auditory stimuli”.
Reticular activation System, RAS
Meet the Reticular activation System, RAS
Reticular means “net or web-like.” The RAS is a net-like formation of nerve cells and their connections lying deep within the brainstem, between the brain and the spinal cord.
Importantly, the RAS is not involved in interpreting the quality or type of sensory input. Rather, it activates the entire cerebral cortex with energy, waking it up, increasing its level of arousal and readiness for interpretating incoming information and preparing the brain for appropriate action.
You will notice in the diagram that specific sensory information comes into the RAS and the outflow goes to the entire cortex of the brain, waking it up and preparing it for the work is has to do.
The RAS is involved in almost everything we do: All learning requires at least a minimal level of arousal in order to attend, concentrate, remember and put learning into memory storage.
The ability to regulate emotions, which often feed into behavioral issues, also depends upon sufficient levels of cortical arousal to inhibit impulses and to control strong emotions. Under-aroused children tend to be fussy, irritable, difficult to manage and are unavailable for learning.
Can iLs enhance the RAS? https://integratedlistening.com/what-is-ils/ The multi-sensory input of iLs has a profound effect on increasing activation of the RAS, thereby increasing the arousal of the entire brain to function optimally and effortlessly. A study by Dr. Sarah Schoen measuring the effect of iLs on arousal levels and auditory processing is currently submitted for publication and provides objective evidence to support what most iLs Associates are well aware of. That is, the iLs program produces positive results related to improved attention, stabilized levels of arousal and the ability to learn and retain information.
Dr. Sarah Schoen’s study on Arousal with the SPD Foundation used both behavioral measures and electrodermal skin response to measure arousal levels in children with Sensory Processing Disorder. Her study found that both under-responsive and over-responsive children achieved normal levels of arousal by the end of a 3-month iLs Program.
Habituation and different severe kinds of Tinnitus
(See also below “orienting Response, Habituation, Locus Coeruleus and RAS”)
Below discuss orienting respons, habituation/dishabituation and Tinnitus in general and in different versions as well as how to find individual biobehavioral tailoring strategies.
Below will be resting on some very interesting work, e.g. https://www.cell.com/current-biology/pdf/S0960-9822(11)00212-0.pdf and https://www.sciencedirect.com/science/article/abs/pii/S0378595515001987 (more below at references!
A Multidisciplinary Tinnitus approach is very complex and not well understood but we can find some superior processes to focus on as well as try to find ways to psychophysiologically measure to get some data for diagnosis as well as outcome measures.
The below picture focus on localisations which can give us ideas how to functionally change assumed dysfunctions into a more normalizing process while used psychophysiological data of direct indirect relevance.
“Following Schaette and Kempter (2006), Schaette and McAlpine (2011) suggested that reduced neural output from the cochlea leads to a compensatory increase in neural gain in the auditory brainstem. The gain could lead to tinnitus due to an amplification of the spontaneous activity of auditory neurons”
Abstract – Dramatic results from recent animal experiments show that noise exposure can cause a selective loss of high-threshold auditory nerve fibers without affecting absolute sensitivity permanently. This cochlear neuropathy has been described as hidden hearing loss, as it is not thought to be detectable using standard measures of audiometric threshold. It is possible that hidden hearing loss is a common condition in humans and may underlie some of the perceptual deficits experienced by people with clinically normal hearing. There is some evidence that a history of noise exposure is associated with difficulties in speech discrimination and temporal processing, even in the absence of any audiometric loss.
There is also evidence that the tinnitus experienced by listeners with clinically normal hearing is associated with cochlear neuropathy, as measured using Wave I of the auditory brainstem response. To date, however, there has been no direct link made between noise exposure, cochlear neuropathy, and perceptual difficulties. Animal experiments also reveal that the aging process itself, in the absence of significant noise exposure, is associated with loss of auditory nerve fibers. Evidence from human temporal bone studies and auditory brainstem response measures suggests that this form of hidden loss is common in humans and may have perceptual consequences, in particular, regarding the coding of the temporal aspects of sounds. Hidden hearing loss is potentially a major health issue, and investigations are ongoing to identify the causes and consequences of this troubling condition.”
https://journals.sagepub.com/doi/10.1177/2331216514550621
More text coming
Autonomic nervous system and Tinnitus
Text coming
How to influence severe Tinnitus with Vagus
(My opinion is perhaps not very common but I believe that focus on only Vagus is not sufficient while we do have to include complex systems interactions, e.g. the autonomic nervous systems, where the sympathetic system is in oscillator relations with the parasympathetic system! In clinical psychophysiology we estimate using Respiratory Sinus arrythmia (RSA) pattern and “size” as point of departure for analysis! In general we need to include the sympathetic–adrenal–medullary axis, a neuroendocrine stress-response system. A stressor is perceived via the sympathetic nervous system, triggering in humans the production and release of hormones such as epinephrine and norepinephrine by the adrenal gland (in particular, the medulla). The SAM interacts chemically with the hypothalamic–pituitary–adrenal axis. Also called sympathetic–adrenal–medullary system; sympathetic adrenomedullary system https://dictionary.apa.org/sympathetic-adrenal-medullary-axis)
Vagus can be influenced in many ways but if you search at internet “profit nudging” prevent you to easily find valuable information while external intervention Vagal implants dominate. (As I describe above) within psychophysiology we e.g. use RSA-biofeedback to see how ANS oscillate and spectral analysis of HR data series to identify e.g. Cardiovagal tone. Below I will only give some examples of how we ourselves can influence Vagal activity.
Another way; Vagus Nerve Stimulation via the Outer Ear Takes Center Stage. Non-invasive vagus nerve stimulation reduces fight-or-flight stress responses. https://www.psychologytoday.com/us/blog/the-athletes-way/201907/vagus-nerve-stimulation-the-outer-ear-takes-center-stage
Or massage; “Massage for Vagus Nerve Stimulation” https://oseamalibu.com/blogs/wellness-blog/massage-for-vagus-nerve-stimulation
More of interests;
“The auricle, or pinna, is the outer part of the external ear that helps to collect sound waves traveling through the air, and direct them into the second part of the external ear, the external auditory canal”. http://diagnosis101.welchallyn.com/otoscopy/educational-topics/anatomy-of-the-ear/?term=cochlea
Above – there are several ”points” or areas behind and ”behind below” the ears that can be influenced via pressure, tapping, massage, … myself, I have found several different variants on site and touch type.
Below in green we can see how the auricular branch of the vagus is located in the outer part of the ear and where may be affected. Is there, for example, different ”tools” for impact BUT can also be done without, i.e. fingers are used to manipulate or one can probably (!) eg. hold for the ears cap and then the inner vibration sound occurs that can (most likely) act as stimulation of vagus that way (Auticulara branch).
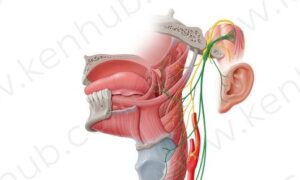 https://www.kenhub.com/en/library/anatomy/the-vagus-nerve
https://www.kenhub.com/en/library/anatomy/the-vagus-nerve
Or ..
Above you can clearly see where stimulation takes place as well as below
Probably more text here about vagus – for several reasons one of which is that it is not easy what I write above – which you will find out when you start trying. Perhaps reasonable understandable knowledge can be a gradual encouragement so everyone can cope and have the energy to ”work”. Clinically, I always worked with patient groups in similar situations to be able to feedback can be given within the group as well!
Swedish texts and pictures in the appendix at http://carism.se/project/projekt-carism/carism-tips/
More text is to come
Psychological interventions, e.g. CBT and biopsychosocial-cultural grounded Tinnitus
As most dysfunctions are multidisciplinary the psychological (spatial-verbal-rational ..) part are more or less taking part of also those dysfunctions which are mainly biological grounded. This means that e.g. behavioral approaches can be part of an integrated interventional toolbox approach. My clinical experiences are that sometimes its contribution is important for a patient’s quality of life but also it can mask biological dysfunction progresses, if too effective.
Concerning CBT in severe Tinnitus (e.g. Hyperarousal Aggressive Tinnitus Syndrome, HATS, a conceptualization I use when it is impossible severe) I do think it is not possible that psychological interventions, how effective they may be, can mask a dysfunctional development BUT it can, as the only offer, prevent clinicians require more substantial their box” intervention toolboxes – which also invite “patients as educated, reasonable competent resources and coworkers in own rehab” (see my argument “But to increase lifestyle related health in humans can only be done thorough learning while doing while understanding while observing while … be motivated by the results related to own doings! That is, mass-education (in Swedish we have a special tradition which facilitated it is use) like we have done clinically for 25 years (based on my dissertation 1986) “patient as educated, competent resource and coworker in her/his own rehabilitation” using a biopsychosocial medicine toolbox. E.g. hypertension patients get happy when they SEE and LEARN (while seeing) what they can to. “Ahhhaaa, that is me doing …. ” can move mountains!” at http://biopsychosocialmedicine.com/paradigm/while-evidenced-based-medicine-is-not-enough-effective/)
Summarizing so far; I do think effective psychological intervention are important per se, but needed to be contextualize into the integrated interventional approach and not separated. Not very easy, but something I do think many psychologists not “fixed in their box” can adjust to. What is needed (if not existing so far?) is real life multidisciplinary, individualized functional manual for both patient and clinicians.
More, independent of reasons for emergence of Tinnitus it is not the first thing that happens to you in your life – you do have a biography, which direct or indirect may interfere, perhaps without no one think about it – or is not clinically considered at all. In my own case, I suffer from PTSD established related to Material Depression (https://en.wikipedia.org/wiki/Maternal_deprivation), which mean that I have to assume that my PTSD is interfering complicating also my present “fight” (severe Tinnitus). Assumed is also tat PTSDs are mor prone to be influenced by Locus Coeruleus based stress (see about this part in this link). On the pother hand (talking about myself now, the personal problems assumed to be associated with my PTSD was the only reason I left music (pianist and conductor) very early to move to biopsychosocial science and clinical work very much influencing my dissertation. Back from personal position to more general, psychological support is probably always important given not believe that it solves everything or it replace anymore concern about biopsychosocial dysfunctions as such we here discuss!
Understanding by reasoning correct, we can expect that any kind of suffering has usually psychological consequences, which in it self can make the dysfunction worse – we can name it nocebo! On the other hand we also can consider biopsychosocial-cultural placebo, a conceptualization not very much understood and which has not got any substantial scientific and clinical interests what I understand from what has happening since 1975 http://biopsychosocialmedicine.com/projects/rd-international-projects-2/placebo-rd/cases/the-1957-placebo-case-the-krebozen-story/ (see more at http://biopsychosocialmedicine.com/projects/rd-international-projects-2/ The huge problem is that Big Pharma has to downgrade placebo-effect to “sugar-pills”-position. I am not the only one arguing that a sound placebo R&D development could be of invaluable benefits for most human health in our world. But as usual profit interests still take care of most of the still reductionistic medicine apparently without any humanistic and political objections).
… will rework the above … especially when it concerns not very severe biological but severe psychological (also based on psychophysiological examinations) expressions of the Tinnitus! Here e.g. CBT can be desicive for effective rehabilitation …
Sense Of Coherence (SOC) and Tinnitus
“Sense of coherence consists of three components ‘comprehensibility’, ‘manageability’ and ‘meaningfulness’ (concept developed by Aaron Antonovsky, 1987 https://www.ncbi.nlm.nih.gov/books/NBK435812/ – https://www.sciencedirect.com/topics/medicine-and-dentistry/sense-of-coherence).
First some personal actual consideration; As my SOC is a part of general health conditions in my clinical paradigm, I personally as well as clinically regard SOC as decisive important (which my contribute to psychophysiological placebo processes, discussed elsewhere – but now only, as I see it placebo tools I use are both spatial and verbal/rational knowledge based ..) in all kinds of biopsychosocial dysfunctions. Such a platform, based on reasonable, well patient adjusted (group) education may enabling “moving” an individual (e.g. patient) from being a passive, perhaps helpless “dependent variable” to become via such applied practical education/communication towards an “independent variable” in line with our manual “patient as an educated, reasonable competent resource and co-worker in own rehab” – continuously upgraded since my dissertation 1986, which is based on George Kelly´s “man as a scientist” https://www.verywellmind.com/george-kelly-biography-2795498 and (https://www.researchgate.net/publication/258488049_Personal_Construct_Theory
Now, after 8 month with extremely hard slowly last month to hard times, I am beginning to see the light of a possible systems complex integrating “diagnosis hypothesis”, which has also consequences on my SOC! Reasons? A reasonable explanation to this hard, not very well understood, symptoms. Also I can more adjust and add strategies into my biopsychosocial toolbox as well as also increase my outcome measure approach. Here SOC contribute obviously towards make my platform more trustworthy.
As Tinnitus often involves permanent, often high pitched alarm cluster, which can not be managed and hard to stand, absence of sense of coherence is a consequence that really should not be underestimated – indeed. Also not knowing what exactly cause it (https://www.signia-hearing.com/blog/dispelling-the-myths-about-tinnitus-and-its-causes/) and “no cure. However, it can be temporary or persistant, mild or severe, gradual or instant. The goal of treatment is to help you manage your perception of the sound in your head. There are many treatments available that can help reduce the perceived intensity of tinnitus, as well as its omnipresence. Tinnitus remedies may not be able to stop the perceived sound, but they can improve your quality of life”. (https://www.healthline.com/health/tinnitus-remedies).
While increasing effort to really understand more and more of different kinds of Tinnitus as well as how to examining and individually treat, psychologists have meanwhile a very important task to support (often very much) suffering individuals to manage their life in general and learning to increase “standing out” what they need to leave out! We can see lack of sense of coherence as a complex biopsychosocial stress factor which not only influence the symptom picture but most of living.
NB psychological support while in parallel work hard with development of scientific and clinical knowledge and its practice – a biopsychosocial focus where understanding of mechanisms also can be a kind of indirect feeling of that Health Care increase in their comprehensibility, manageability and meaningfulness – and the message is “what do not yet understand well the mechanisms behind Tinnitus but we work hard on this as well as how individual interventions can be of increased efficacy”!
More from “(Antonovsky, 1987). Comprehensibility refers to whether or not inner and outer stimuli make sense to us in terms of being coherent, ordered, cohesive, structured and clear. Manageability refers to the extent to which we feel resources are at our disposal to help meet the demands posed by the stimuli to which we are exposed. Meaningfulness refers to whether we can perceive life’s difficulties as ‘welcomed’ challenges worthy of aninvestment of energy, engagement and dedication rather than as a burden that we would prefer to avoid.
Meaningfulness is the motivational component of the concept. In summary, sense of coherence is defined as: a global orientation that expresses the extent to which one has a pervasive, enduring though dynamic feeling of confidence that (1) the stimuli deriving from one’s internal and external environments in the course of living are structured, predictable, and explicable (comprehensibility); (2) the resources are available to one to meet the demands posed by these stimuli (manageability); and (3) these demands are challenges, worthy of investment and engagement (meaningfulness). (Antonovsky, 1987: 19 https://portal.research.lu.se/ws/files/2796842/625628.pdf )
Multidisciplinary Systems Integration
First when I have satisfying recovered from this unanticipated extreme “Inner Burglar Alarms Syndrome”, I can concentrate to try to organize a comprehensive systems synopsis. But right now, I will make a challenging argument “Reductionistic based evidence prevent a reasonable comprehensive multifaceted system integrating clinical work, which meet an individual’s biopsychosocial-cultural every-day life complex situation”. This by many reasons where one is reductionistic methodological paradigms and another rigid reductionistic knowledge explanations in spite of the important work of Guyton and Hall on medical textbook; “Therefore, the principal goal of our Textbook of Medical Physiology has been to try to explain how the different organs and tissues of the body work together, to build in book form this beauty we call ‘‘physiology.’’ At the same time, the same effort has driven us as research physiologists to explore the quantitative field of physiological interrelationships”. https://journals.physiology.org/doi/pdf/10.1152/advances.1998.274.6.S1
More is to come …
Towards an objectification by classification of tinnitus
?? Klassificering av olika Tinnitus varianter/svårighetsgrader
https://www.sciencedirect.com/science/article/abs/pii/S1388245798000340
Mechanisms and classification of tinnitus: a discussion paper https://www.tandfonline.com/doi/abs/10.1080/16513860310017954
Guidelines for the Grading of Tinnitus Severity: The Results of a Working Group Commissioned by the British Association of Otolaryngologists, Head and Neck Surgeons, 1999 https://pubmed.ncbi.nlm.nih.gov/11678946/
https://www.audiologyandhearing.com/the-4-different-types-of-tinnitus/
Diagnostic Approach to Tinnitus https://www.aafp.org/afp/2004/0101/p120.html
Tinnitus is a common disorder with many possible causes. Most cases of tinnitus are subjective, but occasionally the tinnitus can be heard by an examiner. Otologic problems, especially hearing loss, are the most common causes of subjective tinnitus. Common causes of conductive hearing loss include external ear infection, cerumen impaction, and middle ear effusion. Sensorineural hearing loss may be caused by exposure to excessive loud noise, presbycusis, ototoxic medications, or Meniere’s disease. Unilateral hearing loss plus tinnitus should increase suspicion for acoustic neuroma. Subjective tinnitus also may be caused by neurologic, metabolic, or psychogenic disorders. Objective tinnitus usually is caused by vascular abnormalities of the carotid artery or jugular venous systems. Initial evaluation of tinnitus should include a thorough history, head and neck examination, and audiometric testing to identify an underlying etiology. Unilateral or pulsatile tinnitus may be caused by more serious pathology and typically merits specialized audiometric testing and radiologic studies. In patients who are discomforted by tinnitus and have no remediable cause, auditory masking may provide some relief.
Tests/examinations/…
One of the critical problems in all versions of Tinnitus is to reveal what is psychological and what is physiological? And, what about synergies in multifaceted complex interacting in weaved systems/mechanisms/…? Clinical psychophysiology offers some tests which can be of direct or indirect guidance, especially when it concerns dynamic autonomic nervous systems (ANS) related reactions. As many Tinnitus “experience expressions” are not dynamic, which in it self is a, for many, huge problem, but it may even here give some valuable information about what does not happens, e.g. when we do see clear constructive managements of psychophysiological data indicating positive effects on ANS without any subjective experienced expressions of changes in Tinnitus clusters within reasonable time, it indicate that Reticular Activation Systems (RAS) and Locus Coeruleus (LC) is “in charge”, making the intervention often much more complex. Also, here may diagnosed or not PTSD be a complex platform for different Tinnitus problems.
Accordingly, assumed is that very seldom a symptom is not only psychological or physiological based (initially and subsequentially caused/based as well as its complex consequences) but both in ways we at present have limited knowledge/tools/practice .. to uncover/reveal but clinically must assume in some way, not very easy and very responsible …
The expression of pain (I include nowadays “sound pain”) can be very complex indeed, with probably a very complex “message”, which requires as effective as possible biopsychosocial (cultural) examination as possible to at least to some degree encode it.
More about psychophysiology is coming here …
Otoacoustic Emissions (OAEs) https://www.asha.org/public/hearing/Otoacoustic-Emissions/ “There are a number of ways to identify a hearing loss. Each test is used for different people and reasons – Types of Tests – Auditory Brainstem Response (ABR) – Otoacoustic Emissions (OAEs) – Pure-Tone Testing – Speech Testing – Tests of the Middle Ear
Audiometry
http://mayfieldclinic.com/pe-hearing.htm
Our ears have three distinct parts: the outer, middle, and inner ear (Fig. 1). Audiometry tests can detect whether you have sensorineural hearing loss (damage to the nerve or cochlea) or conductive hearing loss (damage to the eardrum or the tiny ossicle bones). During an audiometry evaluation, a variety of tests may be performed.
 Figure 1. The outer ear collects sound waves from the environment and funnels them down the ear canal to the eardrum. Vibrations are made when sound hits the eardrum. Vibrations are passed along tiny bones (ossicles) in the middle ear. The ossicles consist of the malleus, incus, and stapes. The stapes delivers vibrations to the cochlea in the inner ear. The cochlea is a spiral tube filled with liquid and lined with hair cells that are microscopic in size. When the vibration hits the cochlea, it causes the liquid, and subsequently the hair cells, to move. The movement of hair cells generates nerve signals that our brain then understands as sound.
Figure 1. The outer ear collects sound waves from the environment and funnels them down the ear canal to the eardrum. Vibrations are made when sound hits the eardrum. Vibrations are passed along tiny bones (ossicles) in the middle ear. The ossicles consist of the malleus, incus, and stapes. The stapes delivers vibrations to the cochlea in the inner ear. The cochlea is a spiral tube filled with liquid and lined with hair cells that are microscopic in size. When the vibration hits the cochlea, it causes the liquid, and subsequently the hair cells, to move. The movement of hair cells generates nerve signals that our brain then understands as sound.
More – soon …
Intervention overview
Treatment of Tinnitus
https://dizziness-and-balance.com/disorders/hearing/tinnitus/tinnitus_treat.html
About medications
Devices for Tinnitus
Unusual devices advocated for tinnitus
Surgical treatment of Tinnitus
Self help – join American Tinnitus Association
Sugar-pills versions of placebo – see https://dizziness-and-balance.com/disorders/hearing/tinnitus/placebos.html
Tinnitus Remedies – https://www.healthline.com/health/tinnitus-remedies
…” is not a disease — it’s a symptom. It’s a sign that something is wrong with your auditory system, which includes your ear, the auditory nerve that connects the inner ear to the brain, and the parts of the brain that process sound. There are a variety of different conditions that can cause tinnitus. One of the most common is noise-induced hearing loss.
- Hearing aids
- Sound masking devices
- Modified or customized sound machines
- Behavioral Therapy
- Progressive tinnitus management
- Antidepressants and antianxiety drugs
- Treating dysfunctions and obstructions
- Exercise
- Mindfulness-based stress reduction
- DIY mindfulness meditation (DIY = Do It Yourself https://en.wikipedia.org/wiki/Do_it_yourself)
- Alternative treatments as nutritional supplements, homeopathic remedies, acupuncture & hypnosis
None of these treatment options are supported by science. Many people are convinced that the herb gingko biloba is helpful, however large-scale studies have been unable to prove this. There are many nutritional supplements claiming to be tinnitus remedies. These are usually a combination of herbs and vitamins, often including zinc, ginkgo, and vitamin B-12. These dietary supplements have not been evaluated by the U.S. Food and Drug Administration (FDA) and are not supported by scientific research. However, anecdotal reports suggest that they may help some people.”
https://www.healthline.com/health/tinnitus-remedies#tinnitus-remedies
BvS-> We can add s number of additional intervention tools;
Different kind of ways to influence Vagus (implant, Transcutaneous Vagus Nerve Stimulator, massage, ..) e.g. https://www.instructables.com/id/DIY-Transcutaneous-Vagus-Nerve-Stimulator/ and https://www.diytdcs.com/tag/vagus-nerve-stimulation/ and other different kind of stimulation, e.g. …
NB see also introduction to ”How to influence Tinnitus with Vagus” above.
My one biopsychosocial tool box (continuously updated and adjusted to different diagnostic hypothesis problems since my dissertation 1986) will be presented as soon as possible – while still during daily (hopefully, successful) knowledge and practice based refinement.
Meniere’s Disease Diet
Below one of many overviews
https://www.healthline.com/health/meniere-disease-diet#other-treatment
Meniere’s disease has no known cause or cure. However, with the right treatment — which often includes diet and supplements — you can manage the most debilitating aspects of the condition.
Meniere’s disease is dependent on the body’s fluid and blood system.
A diet for managing this condition should focus on:
- eliminating substances that cause the body to retain water
- introducing more diuretics to reduce fluid volumes in the body
- limiting harmful substances that constrict blood flow
- limiting dietary supplements and common substances that worsen symptoms of Meniere’s disease
Water and diuretics
Water retention makes Meniere’s disease worse, but this doesn’t mean you should stop drinking fluids. It’s more important that you avoid fluids that contain large amounts of sugar and salt, such as soda or concentrated juices, which make you retain water.
Instead, drink the following fluids evenly throughout the day:
Diuretics are an important part of managing Meniere’s as well.
Diuretics are drugs that make the kidneys produce more urine, which reduces the volume, salt levels, and fluid pressure in the body. These reductions help you to better manage your condition.
Some common diuretic drugs prescribed for Meniere’s disease include:
- chlorthalidone (Thalitone)
- furosemide (Lasix)
- Side effects of using diuretics can include:
- low blood pressure (hypotension)
- weakness
- cramps
- dehydration
Limit salt and sugar intake
Foods with a high sugar or salt content cause water retention, which can worsen symptoms of Meniere’s disease.
Sugar prompts an insulin response from the body, and insulin retains sodium. Sodium causes the body to retain water.
Try to avoid foods with concentrations of simple sugars, such as:
- table sugar
- honey
- high-fructose corn syrup
- candy
- chocolate
- Instead, focus on foods with higher levels of complex sugars, such as:
- legumes, like nuts, beans, and lentils
- whole grains
- brown rice
- sweet potatoes
The same rule applies to salt intake. It’s difficult to cut back on sodium because so much of our Western diet is packed with salt.
However, people with Meniere’s disease should aim for less than 2,300 milligrams of sodium each day, according to the Mayo Clinic.
Intake should be spread evenly throughout the day. Much more than that will cause water retention.
Foods naturally low in sodium include:
- fresh fruits and vegetables
- unprocessed grains
- fresh meats, poultry, and fish
Refrain from alcohol, tobacco, and caffeine
Caffeine should be avoided because it’s a stimulant and can make tinnitus louder.
Caffeine and alcohol also interfere with your body’s ability to regulate fluid levels, which can make the inner ear worse, causing headaches, pressure, and vertigo.
The nicotine in cigarettes and other tobacco products can constrict the blood flow to the inner ear, making all symptoms worse. It’s better to avoid nicotine and tobacco altogether if you have Meniere’s disease.
Over-the-counter (OTC) medications
Aside from medications your healthcare provider prescribes, certain OTC medications and supplements can help or hinder symptoms of Meniere’s disease.
Beneficial OTC medications
Common effects of Meniere’s disease and vertigo are:
- dizziness
- nausea
- motion sickness
Some medications that can help relieve these symptoms are:
- anti-nausea medication, like Dramamine
- antihistamines, like Benadryl
Dramamine is helpful because it helps prevent:
- dizziness
- motion sickness
- nausea
Swelling in the ear can also contribute to vertigo. Taking anti-inflammatory drugs occasionally can be helpful.
Reducing swelling in the ear will curb nausea and dizziness associated with vertigo.
Harmful OTC medications
At the same time, there are common OTC drugs you should avoid because they interfere with Meniere’s disease.
Try to avoid the following:
Antacids are packed with sodium, which will cause water retention.
Drugs like ibuprofen (Advil, Motrin), which is an NSAID, can also cause water retention and interfere with electrolyte balance. An electrolyte balance is important for the regulation of inner ear fluid.
According to the Vestibular Disorders Association, Aspirin can worsen the symptoms of tinnitus.
Other treatment options
Changing your diet is a simple, inexpensive way to help relieve Meniere’s symptoms at home.
However, if a new diet doesn’t work, your healthcare provider may also recommend medication or surgery to help treat your condition.
Prescription medication
Vertigo is the most common and most debilitating aspect of Meniere’s disease. Your healthcare provider may prescribe medication to help reduce and manage this symptom and others.
Benzodiazepines like diazepam (Valium) or lorazepam (Ativan) can be used to shorten an episode of symptoms.
Anti-nausea medications like promethazine or meclizine can be used to treat and manage the nausea and vomiting associated with vertigo.
Surgery
Surgery is usually only a treatment option for Meniere’s disease when all other treatments haven’t worked.
Surgery is primarily used to eliminate debilitating episodes of vertigo. Surgery options include decompressing fluid in the inner ear or cutting a nerve to permanently cure episodes of vertigo.
Living with Meniere’s disease
While there’s currently no cure, Meniere’s disease can be effectively managed, allowing people with this condition to live a satisfying and full life.
A healthy diet and working with your healthcare provider to create an informed approach to medication and other treatment options can help improve your outlook.
Last medically reviewed on January 16, 2020
Swedish activities/examinations/interventions/presence of different types of Tinnitus in the population
Interesting link I just observed: https://ki.se/forskning/forskaren-tinnitus-uppmarksammas-inte-tillrackligt (will ask for permission to translate it)
Text coming
My case
More and more approaching a possible diagnosis hypothesis;
- First cochlea dysfunctions associated with Secondary Endolymfatic Hydrops, (see that heading above), which is related to high sensitivity in terms of symptom change associated with changes in air pressure. Causes may be more than one, e.g. associated with systemic inflammation, head trauma, … and also possible imbalance in neurotransmittors related to GABA deficit. ”The build-up of fluid in the inner ear can be caused by trauma (injury) or inflammation. SEH can happen weeks, months or even years after the trigger that caused it. If SEH happens long after a disease, it is known as delayed SEH.” https://balanceanddizziness.org/disorders/vestibular-disorders/secondary-endolymphatic-hydrops/Given Endolymfatic Hydrops, it is important to understand how drainage function or not associated with an Eustachian Tube Dysfunction (see that heading above). For me this can explain while the longer I sleep the more towards “Exploding Head Syndrome”, EHS (in my version long-termed sizzling-blasting)- this while the tube is closed during sleep (or laying straight). First 6 month I had to sleep (almost) sitting! As there are probably also an imbalance in neurotransmitter balance which I have worked with for 5 month now, improvement to laying straight up to two hours without increased “alarm clusters”. Complicating, if the Eustachian Tube if a tube can’t open, fluid can get trapped in the middle ear but if it is close or patulous, the Eustachian tube becomes stuck in the open position it will be another type of objective tinnitus as well as open for mucus inflow from throat, nose.. and inflammations may be developed in the Eustachian tube and the Cochlea. I work more on both focuses!My increased blood pressure at EHS may be related to resting Sympatico-Adrenal-Medulla activity during REM-sleep, with too much when it reactivates. also cortisol is involved https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2902103/ + https://www.naturalmedicinejournal.com/journal/2010-06/role-cortisol-sleep – as well as
Interactions between sleep, stress, and metabolism: From physiological to pathological conditions https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4688585/ where sympathetic stress activation during dreams may not be neglected.
- Then Spine based, e.g. associated with my head trauma, foraminala cervikal and lumbal stenosis while e.g. “Neck inputs can modulate brainstem structures that are involved in sound generation” https://www.dizziness-and-balance.com/disorders/hearing/tinnitus/cervical%20tinnitus.htm and “Tinnitus can be triggered by cervical neck instability, TMJ-TMD can be triggered by cervical neck instability. Tinnitus can be caused by temporomandibular disorders” .. “something is missing, in a tinnitus examination. It is a look at the neck” https://www.caringmedical.com/prolotherapy-news/tinnitus/
- As well as in general problem/symptom complication based on my early initiated PTSD (established during early first year, associated with Material Depression (https://en.wikipedia.org/wiki/Maternal_deprivation – very clear symptoms), which is assumed to be associated with SAM (Sympatico-Adrenal_Medulla) and here especially Locus Coeruleus reactivity, which can not be controlled by biofeedback usually). NB PTSD early is developed in a not mature brain! (Something I have worked with since 1975 and later used as one of the tool in my manual in my dissertation 1986).
As the above is not possible to in detail examine, it is based on limited but still acceptable knowledge based. What is really needed to know more of is (a) about probable GABA deficit, (b) Secondary Endolymfatic Hydrops (via intervention?) and cervikal influences, where also inflammation can be a part of the process.
Self-treatment, so far, is a biopsychosocial program/toolbox where particularly (i) low-dose Oxascand and GABA (2 x 250 mg) supplement interplay and (ii) 40 minutes Beta-Endorphine exercise (following my dissertation manual) as well as (iii) Autophagy (16-18 fast/day) can right now be mentioned.
Thus, more tools (tailoring my biopsychosocial toolbox) I have used are described elsewhere.
For me, except hard to stand that the Burgler Alarm High Pinched Sound Knives has Lack of Sense of Coherence (see above “Coherence and Tinnitus), which has been and is very hard to stand – motivating me to try to work within a, for me, new complex, multifaceted, and not well understood field to try to increase my Sense of Coherence, in terms of knowledge and hypotheses development as well we its applications – as well as the apparently (lack or at best much limited) ditto in clinical science and practice.
One thing I try to understand and do something to change is vertigo – all the time I have very moderate which I have learn to cope with but during the night (I sleep very well 8 hours at least with 4-6 interruption but if more than 3 hours at a time (a) Vertigo increase so I can hardly more to rest room even with a crutch and (b) alarm is increasing quite to very very much, not “exploding head syndrome but “a long explosive feeling” which can go on for, at worsted, hours. I suspect micro-circulation during sleep complicating Cochlea Dysfunctions as Secondary Endolymfatic Hydrops. (Hope I) Am approaching a solution to make it less hard. Can below update when I solved it, while others can get ideas how to do with such own symptoms.
My message to Tinnitus colleagues
Below(above inte ”my Case” your may also get some info of you for you) I write somewhat personal about what perhaps others could have use of
First, as I see it, it is not very easy for others without Tinnitus to understand how impossible it can be for some of us – but also quite or not very hard suffering need to be respected. I believe that many define/associate/understand the word Tinnitus as “soft ear hum”, which it can be. I had that kind of soft ear hum” in 60 year when suddenly extreme four inner “alarm” emerged, and still is not yet well recovered (more elsewhere about all what I have done)
External factors can influence your inner sounds, e.g. I, as many others (but which perhaps do not know it) am very sensitive to air pressure and humidity changes as well as very low stable levels (see “Whether and Tinnitus” above).
Much more text is coming ….
If anyone will write something mail to info@stressmedicin.se
Main recerences:
http://www.cochlea.eu/en
https://www.sciencedirect.com/science/article/abs/pii/S0378595515001987
https://teachmeanatomy.info/neuroanatomy/pathways/auditory-pathway/
http://www.robertshearingclinic.com/tinnitus-explained-landing-page
https://www.researchgate.net/figure/The-human-auditory-system-A-cross-section-of-the-ear-B-Cross-section-of-the-cochlear_fig5_320077050
https://www.frontiersin.org/articles/10.3389/fpsyg.2019.01153/full
https://www.frontiersin.org/articles/10.3389/fpsyg.2019.01153/full
More is to come …