2022-02-22 – ?? NB, I am writing with a severe kind of (hard to deal with) blasting sound symptoms (permanent since 2,5 years, no habituation at all but dishabituation and orienting responses constant, something the evolution is not prepared for – and have no strategies for) may influence the below! More about symptoms at http://carism.se/2021-22/personal-clinical-situation/ – am used with manageable tinnitus since 60 years.
2022-03-12 Actual summary of the first picture below (Swedish just under this summary):
The working hypothesis is that the causes of my very difficult-to-manage symptoms are systemic inflammaging (SIA, prolonged, gradual, during increasingly dysfunctional development) in several ways creating severely identifiable low-grade inflammations that, among other things, increase spinal dysfunction (cause of head trauma accident, see MRI interpretations of data, which are likely to form the ”main engine” of an complex integrated symptom development, like, (except see above), swollen nose and throat, teary eyes, as well as spinal problems, especially night). Overall, this affects the complex system picture where even Cochlea’s impact by complex InflammAging may increases my 60-year manageable noise damaged tinnitus (see (https://www.researchgate.net/publication/353370940_Neuroinflammation_and_Tinnitus). Increased significant symptoms in which the permanent, severe sound symptoms covariate with the spinal ones, pointing to non-well-aerated cavities and possibly hypoxi – working with complex self-care multifaceted toolbox – will updates the development below…
Svenska: 2022-03-12 Sammanfattning av första bilden nedan:
Arbetande hypotesen är att orsakerna till mina mycket svårhanterliga symptom är systemisk Inflammaging (SIA, långvarig, gradvis under allt mer dysfunktionell utveckling) på flera sätt skapar svår identifierbara låg gradiga inflammationer som bl.a. ökar spinala dysfunktionen (orsak huvudtrauma olycka, se MRI tolkningar av data, som sannolikt utgör ”huvudmotorn” i en integrerad komplex symptomutveckling, som, (förutom se ovan), svullen näsa och hals, tåriga ögon, samt ryggproblem, speciellt natt). Sammantaget påverkar detta komplexa systembilden där även Cochlea påverkan av komplext InflammAging kanske ökar min 60-åriga hanterbara bullerskade tinnitus (se (https://www.researchgate.net/publication/353370940_Neuroinflammation_and_Tinnitus). Ökade signifikanta symptom där de permanenta, svåra ljudsymptomen samvarierar med de spinala, vilket pekar mot icke-väl luftad hålighet och ev. hypoxi – arbetar med komplext åtgärds verktygslåda – kommer att uppdatera utvecklingen nedan …
Below is an integrated overview of possible dysfunctional sources associated with my complex dysfunctions. As there are around 40-50 different “constellations” of sources of tinnitus (see https://carism.se/projekt-carism/a-multidisciplinary-overview-of-the-tinnitus-syndrome-fields/overview-of-some-of-the-tinnitus-syndrome-approaches/ urgent needed is had work to try to understand multifaceted systems integrating (synergy to not forgotten), while often it is not ONE sources! Below I try, based on the nature of my symptoms (trying to distinguish what is subjective generated additions), to develop a working spatial approach with also trying to add some explanatory verbalizations.
The picture below will gradually (I hope) be updated and more understandable
(please click at the ”box”)
 NB, about how the Limbic systems functions can interfere in the picture above, see http://carism.se/2021-22/multifaceted-hypothesis-overview/about-my-paradigm-on-limbic-and-neocortex-integration-in-human-brain/- and for a broad multidisciplinary overview see http://carism.se/projekt-carism/a-multidisciplinary-overview-of-the-tinnitus-syndrome-fields/overview-of-some-of-the-tinnitus-syndrome-approaches/
NB, about how the Limbic systems functions can interfere in the picture above, see http://carism.se/2021-22/multifaceted-hypothesis-overview/about-my-paradigm-on-limbic-and-neocortex-integration-in-human-brain/- and for a broad multidisciplinary overview see http://carism.se/projekt-carism/a-multidisciplinary-overview-of-the-tinnitus-syndrome-fields/overview-of-some-of-the-tinnitus-syndrome-approaches/
NB, see also updated links on NonTubercle Mycobacteria and increased consensus of its presence in bone, tissue, … spondylitis, RA, … at NonTubercle Mycobacterium | BOAIM2: Bergvik Open Academia for Innovative Medicine Management and sub pages.
NB also that GERD also include exclusion of Barett´s syndrom (motivated to examine motivated by many years with GERD symptoms)
First, I will comment the above quite complex picture. After 2,5 years, it seems I can now connect apparently independent symptoms – “Seemingly unrelated symptoms in the head and neck region are eliminated when a patch is applied on specific locations on the Tympanic Membrane” https://www.frontiersin.org/articles/10.3389/fneur.2020.00014/full – I have in the pictures above included some of my symptoms (NB, as I feel astonishing well in spite of very hard blasting symptoms, most is probably neurobiological, were the hardest most likely is a synergy of some of the above mentioned)
Among some, not very hard symptoms are (a) balance problems, very little, but still, (b) breathing through the right eardrum (not functional), (c) nose swollen (– right nostril Basaliom Glass type 3 surgery October 2017) during sleep and inactivity and Toynbee indication of internal pressure problems, (d) watery eyes (movement related), (e) air pressure changes (e.g. also revealed via Toynbee maneuver), (f) not always silent refluxes, (g) eye symptoms (according to some physicians) associated with silent migraine. A lot, but manageable while the very hard one’s override all of them.
A question is, why so many? One answer may be associated with Systemic InflammAging (SIA), low graded, cytokine molecule age changes (e.g. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5900450/ + https://www.frontiersin.org/articles/10.3389/fimmu.2018.00586/full but a second, an additional source may be the injuries from my head trauma accident ( (see MRI, at “neighbor” page), which gradually deteriorate, cramped for efferent and afferent signals, where orthopedist Bengt Sturesson argues decompression of the L5 nerve left as influential. The left fits well with the most severe 2.5-year left-side permanent symptom. Perhaps adding also, Aggressive Prostate cancer radiation treatment (www.docrates.com – Helsinki) June – October 2018.
-> BUT! They are both (above) probably synergy integrated (destructively) partly complies with “Inflammaging determines health and disease in lumbar discs-evidence from differing proteomic signatures of healthy, aging, and degenerating discs” https://pubmed.ncbi.nlm.nih.gov/31125691/ See more the link, e.g. ”The true understanding of aging and disc degeneration (DD) is still elusive. MRI has not helped our attempts to understand the health and disease status of the discs as it reflects mainly the end morphologic changes and not the changes at a molecular level.”
Below details is listed (no yet completed – takes time … but coming)
A: Limbic memory construct cluster reconsolidation continuously updating (mutually) means internal and external processes are internalized, of quite much not consciously observed but its consequences/results can we sometimes be consciously aware of. The concept “state dependent learning” (including not conscious) function as reconsolidation in both directions (updating memory constructs as well as interfere with present state). This means that most (all?) physiological processes charge our spatial (Limbic) and verbal (neocortex)(see Cultural evolution of human brain based on our (very much modified interacting with) mammalian and reptilian brains … | Cultural Medicine) = there are mostly psychophysiological processes even when it looks like either of them! Consequences? Interventions need to be addressing both = psychophysiological integrated tools!
B: ”Non-tuberculosis mycobacteria (NTM)
NB, see also updated links on NonTubercle Mycobacteria and increased consensus of its presence in bone, tissue, … spondylitis, RA, … at NonTubercle Mycobacterium | BOAIM2: Bergvik Open Academia for Innovative Medicine Management and sub pages.
BvS there are 190 ”versions”) increases in incidence. It is environmental-related, acid-fast bacillus that causes cutaneous infections mainly after TRAUMA (BvS as mine), surgery.. The skin’s ”expression” includes abscess, sporotrichoid nodules or ulcers, but also less distinctive signs. Important species include Mycobacterium marinum and rapidly growing mycobacteria: M. fortuitum, M. abscessus and M. chelonae. Getting tissue for mycobacterial culture and histopathology helps diagnosis. Optimal therapy is not well established, but is species dependent and is generally dictated by sensitivity studies. Treatment often includes the use of several antibiotics for several months and the potential use of additional surgery. https://pubmed.ncbi.nlm.nih.gov/26143432/
Previously had (slightly) burning skin on the upper body, face, strangely ”jumping processes”, mostly on the face (and swollen nose and throat. Some US doctors work/publish about the above, some atypical problems. My symptoms have now returned. Well recognized. See now also that the above can possibly be linked to InflammAging (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6777092/) and also in some cases to tinnitus (https://pubmed.ncbi.nlm.nih.gov/28947034/). Could it be a contributing factor even to my 2.5 years of severe still permanent sound alarm hard problems/symptoms?
What Are Mycobacterium Avium Complex (MAC) Infections? Causes, Treatment, Prevention, and More https://www.everydayhealth.com/rare-diseases/mycobacterium-avium-complex-infections/ “ Signs of pulmonary mycobacterium avium complex (MAC) infections start slow and gradually get worse over time .. Symptoms of disseminated mycobacterium avium complex infections can include: Symptoms: Fever, Sweating, Fatigue, Weight Loss, Diarrhea, Shortness of breath, Abdominal pain, Anemia … https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7881820/ ”.. NTM may also present as localized disease involving extrapulmonary sites such as lymph nodes, skin and soft tissues and rarely bones. .. Rapid molecular tests are now available for confirmation of NTM diagnosis at species and subspecies level.”
C: EMF – Electromagnetic Field: EMF-data shows that I react (measured first after longer period of laptop use, which was associated with odd symptoms – then I measured with EMF-measurement equipment showing while I reacted). But probably not main reasons for my complex symptoms. Can also be a ”side effects” associated with influence due to neurological functioning associated with cervical dysfunctions? More info at EMF-Quantum medicine | Quantum Medicine
D: Locus Coeruleus overactivity after REM sleep may also substantially influence potential “Silent reflux, also known as laryngopharyngeal reflux (LPR), is a condition in which stomach acid flows back up the esophagus (swallowing tube) into the larynx (voice box) and throat. LPR is called silent reflux because it often does not cause any symptoms in the chest” https://utswmed.org/conditions-treatments/silent-reflux/. LC (and SAM) influence the sphincter to become dysfunctional (increase LC/SAM increase sphincter dysfunctions). Summarizing, not functional LC have two influences in the hypothesis.
LC is particular important in my case. Since first year in life, I have had problems with LC (PTSD) but also its “treat-mentor”, while evolution has a treat-mentor , the beta-endorphin system, which can be activated behaviorally. This means I still can use this evolutionary provided skill.
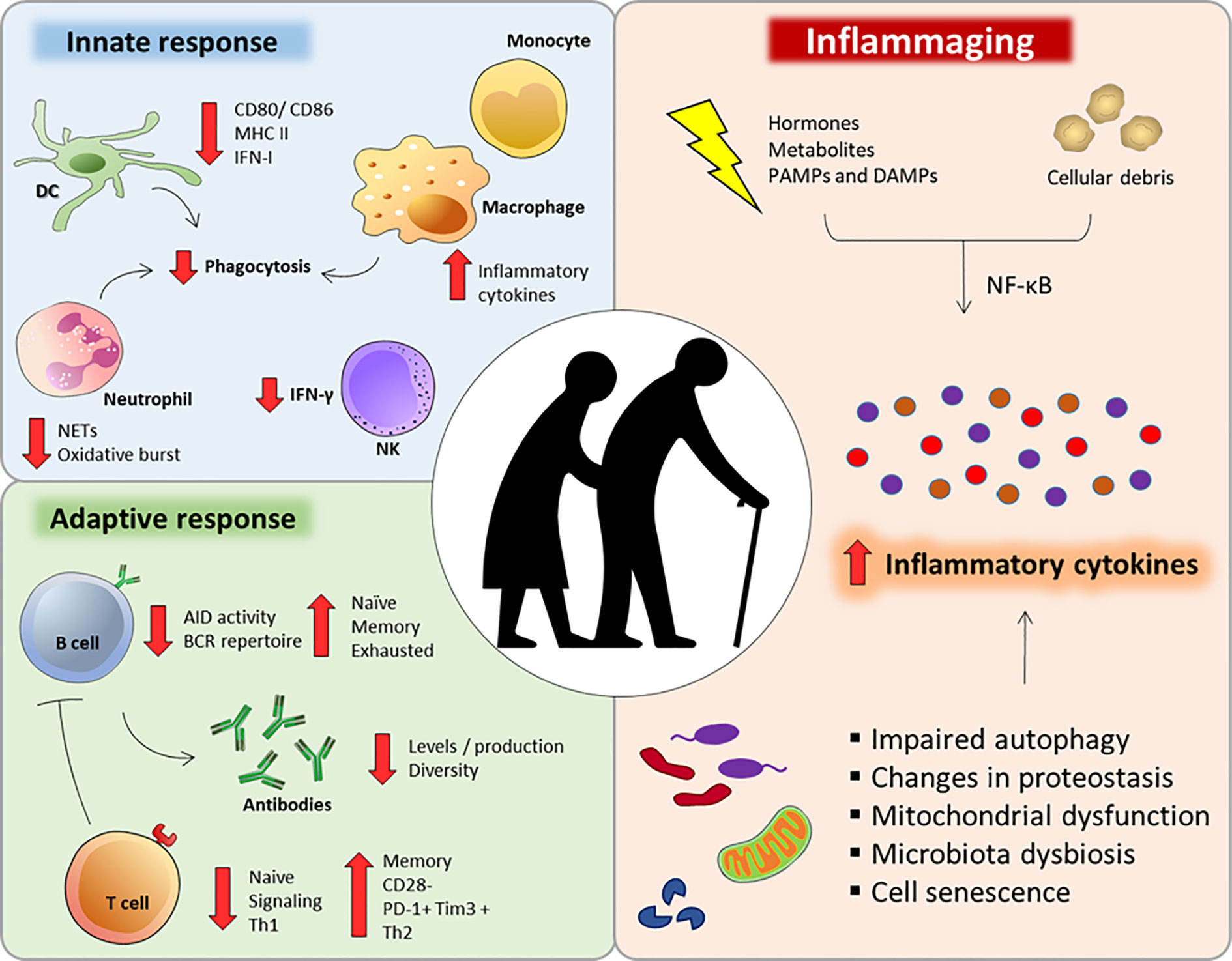
E: InflammAging
More info at Senoinflammation or Inflammaging or …??? | Biopsychosocial Medicine and InflammAging in general and local .. | Quantum Medicine (and sub page)
InflammAging (Claudio Franceschi, 2000) has, tanks to recent knowledge development, become importantly be considered: ”Inflamm-aging (also known as inflammaging or inflamm-ageing) is a chronic, sterile low-grade inflammation that develops with advanced age, in the absence of overt infection, and may contribute to clinical manifestations of other age related pathologies. Inflammaging is thought to be caused by a loss of control over systemic inflammation resulting in chronic, overstimulation of the innate immune system. Inflammaging is a significant risk factor in mortality and morbidity in aged individuals [2] ..
Current research studying inflammaging is focused on understanding the interaction of dynamic molecular pathways underlying both aging and inflammation and how they change with chronological age.” https://en.wikipedia.org/wiki/Inflammaging
But importantly->Inflammaging determines health and disease in lumbar discs-evidence from differing proteomic signatures of healthy, aging, and degenerating discs https://pubmed.ncbi.nlm.nih.gov/31125691/ “.. discs” https://pubmed.ncbi.nlm.nih.gov/31125691/ See more the link, e.g. ”The true understanding of aging and disc degeneration (DD) is still elusive. MRI has not helped our attempts to understand the health and disease status of the discs as it reflects mainly the end morphologic changes and not the changes at a molecular level.” … Conclusions: Our study documented diverse proteome signatures between the young, aging and degenerating discs. Inflammaging was the main differentiator between normal biological aging and DD (disc degeneration). Clinical significance: Multiple inflammatory molecules unique to DD were identified, allowing the possibility of developing specific biomarkers for early diagnosis and thereby provide evidence-based metrics for preventive measures rather than surgical intervention and also to monitor progress of the disease.”
Inflammaging: Age and Systemic, Cellular, and Nuclear Inflammatory Biology in Older Adults https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6777092/ “STAT signal transducer and activator of transcription … Within a community-dwelling sample of older adults, older age is associated with increases in STAT activation, along with increases of systemic inflammatory cytokines. In older adults, heterogeneity in age-related increases in inflammatory disease risk may be related to individual variability in inflammation”
Source of Chronic Inflammation in Aging
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5850851/
“Aging is a complex process that results from a combination of environmental, genetic, and epigenetic factors. A chronic pro-inflammatory status is a pervasive feature of aging. This chronic low-grade inflammation occurring in the absence of overt infection has been defined as “inflammaging” and represents a significant risk factor for morbidity and mortality in the elderly. The low-grade inflammation persists even after reversing pro-inflammatory stimuli such as LDL cholesterol and the renin–angiotensin system (RAS). Recently, several possible sources of chronic low-grade inflammation observed during aging and age-related diseases have been proposed. Cell senescence and dysregulation of innate immunity is one such mechanism by which persistent prolonged inflammation occurs even after the initial stimulus has been removed. Additionally, the coagulation factor that activates inflammatory signaling beyond its role in the coagulation system has been identified. This signal could be a new source of chronic inflammation and cell senescence. Here, we summarized the factors and cellular pathways/processes that are known to regulate low-grade persistent inflammation in aging and age-related disease.”
Conclusion: “Ideally, inflammation should subside immediately after elimination of the pathogen and insult to allow normal tissue to be rebuilt. However, low-grade persistent inflammation occurs in the majority of older people, leading to degeneration of several organs. There is strong evidence that the development of age-related multi-factorial conditions such as cancer, cardiovascular disease, Alzheimer’s disease, type II diabetes, frailty, sarcopenia, and osteoporosis is associated with low-grade elevations of circulating inflammatory mediators. Considering that aging is a complex process that results from a combination of environmental, genetic, and epigenetic factors, focusing future work on interventions addressing selectively destroying senescent cells, namely, “senolytic therapies” in the aging host rather than by treating symptoms of disease or attempting to block the effects of the multi-source of inflammaging, will offer improved therapeutic opportunities (49–52).
Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6146930/
“Most older individuals develop inflammageing, a condition characterized by elevated levels of blood inflammatory markers that carries high susceptibility to chronic morbidity, disability, frailty, and premature death. Potential mechanisms of inflammageing include genetic susceptibility, central obesity, increased gut permeability, changes to microbiota composition, cellular senescence, NLRP3 inflammasome activation, oxidative stress caused by dysfunctional mitochondria, immune cell dysregulation, and chronic infections. Inflammageing is a risk factor for cardiovascular diseases (CVDs), and clinical trials suggest that this association is causal. Inflammageing is also a risk factor for chronic kidney disease, diabetes mellitus, cancer, depression, dementia, and sarcopenia, but whether modulating inflammation beneficially affects the clinical course of non-CVD health problems is controversial. This uncertainty is an important issue to address because older patients with CVD are often affected by multimorbidity and frailty — which affect clinical manifestations, prognosis, and response to treatment — and are associated with inflammation by mechanisms similar to those in CVD. The hypothesis that inflammation affects CVD, multimorbidity, and frailty by inhibiting growth factors, increasing catabolism, and interfering with homeostatic signalling is supported by mechanistic studies but requires confirmation in humans. Whether early modulation of inflammageing prevents or delays the onset of cardiovascular frailty should be tested in clinical trials.”
The role of nutrition in inflammaging https://www.sciencedirect.com/science/article/pii/S1568163722000381
- Inflammaging, a low-grade, chronic, sterile inflammatory state occurs in the elderly.
- Inflammaging contributes to the pathogenesis of ageing and age-related diseases.
- Nutritional status is critical for maintaining proper immune system functionality.
- Diet has a direct influence on inflammation and can counteract inflammaging.
- Intake of whole grains, vegetables, fruits, nuts and fish can decrease inflammation.
“Conclusions: Dietary components may affect inflammation directly, counteracting the low grade age-related inflammation. In this regard, healthy diets, including the Mediterranean diet, are associated with lower concentrations of inflammatory mediators, like C-reactive protein (CRP) and Tumor Necrosis Factor-α (TNF-α), that are hallmarks of inflammaging. Among the components of a healthy diet, a higher intake of whole grains, vegetables and fruits, nuts and fish are all associated with lower inflammation. One area of promising research is the microbiome-ageing interaction. Indeed, dysbiosis plays a role in sub-optimal metabolism, immune function and brain function and contributes to the poor health and impaired well-being associated with ageing. Modulation of the gut microbiota has shown promising results in some disorders. Additionally, the discovery of several molecular pathways associated with ageing, and the characterization of the beneficial effects of calorie restriction (CR) in modulating metabolic pathways and preventing inflammation, should encourage research on CR mimetics, drugs able to promote lifespan and extend healthspan.”
Age-related cerebral small vessel disease and Inflammaging https://www.nature.com/articles/s41419-020-03137-x
“Circulating biomarkers of CSVD (cerebral small vessel diseases) inflammation were classified as markers of systemic inflammation and markers of vascular inflammation/endothelial dysfunction6. Besides, four core MRI features have been identified as imaging markers of CSVD, namely white matter hyperintensities (WMH), lacunae, cerebral microhemorrhage (CMB), and perivascular space enlargement (EPVS)56.” … The regional analysis showed blood markers of vascular inflammation are often associated with deep perforating arteriopathy (DPA), while blood markers of systemic inflammation appear to be associated with cerebral amyloid angiopathy (CAA). Here, we discuss recent findings in the pathophysiology of inflammaging and their effects on the development of age-related CSVD. Furthermore, we speculate the inflammaging as a potential target for future therapeutic interventions to delay or prevent the progression of the age-related CSVD.
Fig. 1: The deep interactions between aging, inflammaging, and age-related CSVD.
As aging, several cellular and molecular mechanisms lead to chronic inappropriate activation of the immune system. This complex interaction between genetic susceptibility and risk stimuli (both exogenous and endogenous) contributes to the continuous activation of a limited range of confounding sensors which triggers inflammaging (upper part of the box). The resulting synthesis and release of different inflammatory mediators are related to the common pathophysiological mechanisms of age-related diseases. For age-related CSVD, regional analyses showed that blood markers of vascular inflammation were associated with deep perforating arteriopathy (DPA), while blood markers of systemic inflammation were associated with cerebral amyloid angiopathy (CAA), both of which were closely related to the critical pathophysiological mechanisms of blood-brain barrier leakage and endothelial dysfunction (lower part of the box).”
InflammAging & Tinnitus
Neuroinflammation mediates noise-induced synaptic imbalance and tinnitus in rodent models https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3000307 “…This excitatory-to-inhibitory synaptic imbalance was completely prevented by pharmacological blockade of TNF-α expression. These results implicate neuroinflammation as a therapeutic target for treating tinnitus and other hearing loss–related disorders.”
Chronic Inflammation – Inflammaging – in the Ageing Cochlea: A Novel Target for Future Presbycusis Therapy https://www.researchgate.net/publication/320354252_Chronic_Inflammation_-_Inflammaging_-_in_the_Ageing_Cochlea_A_Novel_Target_for_Future_Presbycusis_Therapy
Neuroinflammation and Tinnitus
https://pubmed.ncbi.nlm.nih.gov/34282564/
” Neuroinflammation is the central nervous system’s response to: injury, infection, and abnormal neural activity. Inflammatory processes are known to mediate many diseases, and recently evidence indicates that neuroinflammation underlies hearing disorders such as presbyacusis, middle-ear disease, ototoxicity, noise-induced hearing loss, and tinnitus. This chapter provides a review of the role of neuroinflammation in the etiology and treatment of tinnitus. Specifically, our research team has demonstrated that both tumor necrosis factor alpha (TNF-α) and calpain signaling pathways are involved in noise-induced tinnitus and that blocking them yielded therapeutic effects on tinnitus. Other efforts such as controlling acute inflammatory response via specialized pro-resolving mediators may help provide insight into preventing and treating tinnitus-related inflammatory processes”.
More of interests?
https://cmb.i-learn.unito.it/pluginfile.php/5044/mod_resource/content/1/Minciullo_et_al.pdf
https://www.mdpi.com/2073-4409/11/3/359/htm
https://rmdopen.bmj.com/content/rmdopen/7/1/e001470.full.pdf
https://www.frontiersin.org/articles/10.3389/fimmu.2020.579220/full
& https://immunityageing.biomedcentral.com/articles/10.1186/s12979-020-00196-8
F: Problems in eardrum and with nasal breathing
Eardrum
Strange symptoms related to the eardrum that may indicate;
- Cholesteatoma is an abnormal, noncancerous growth that forms behind the eardrum. Cholesteatomas can become large enough to affect hearing and increase your risk of other serious conditions. https://my.clevelandclinic.org/health/treatments/21535-cholesteatoma
- Perforated eardrum: “A hole or rupture in the eardrum .. The causes of a perforated eardrum are usually from trauma or infection .. loss of hearing can be great and tinnitus (ringing in the ear) may be severe. .. Chronic infection as a result of the perforation can cause persistent” symptoms https://earnosethroatmed.com/perforated-eardrum
Observations:
- During back-neck massage, a new type of tinnitus sound occurs, BUT only im left ear – pulsating with massage “basic rhythm” in the form of pulsating pinging sounds, only in the left ear (affecting the eardrum likely), with gradually slowly habituates!
- Just when my ears ”pass” the water surface, a clinic in the eardrum takes place just as at the Toynbee Maneuver (TM)! Thus, unlike the Valsalva maneuver (where the eardrum is affected via Eustachian tube), TM affects muscles(s) via swell muscles(s). In addition, I can do TM without holding for the nose (which is the original method, which suggests that the functioning of the nose is not completely ok. My guess is that it is the second clam (and ostemeatal complex) where it is not free (and not fully air-conductive resulting in mild hypoxia) passage that causes great sensitivity to air pressure changes. However, probably not enough to cause it. The above is just a part of for me unusual reactions, e.g. massage circles around other nasal clam and double chin movements produce similar movements in the eardrum.
There are more observations related to the above:
- From Physician observations: “Inspecting both ears, in the right ear there is a thick trabekel across the ear canal from about 10 o’clock to 5 p.m … In left ear I see an eardrum that has scars, striped earwax, when I suck it off, it comes out skin-colored tissue (exostosis). The patient “has not without remarks canals and eardrum” (my comment while a little difficult to translate). I wonder if this is the basis for the patient’s tinnitus problems and if there is a possible cholesteatoma behind it”
- Moreover, in international references discusses, e.g. “Ear children get also problems as adults” “Association Between Childhood Hearing Disorders and Tinnitus in Adulthood” https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2468493 may be inte lines with my hard ear infections 1944 ..
Nose
See also ”4” just above!
Swollen nose during sleep/lying inactivity clearly affects the Toynbee phenomenon. The above also seems to relate to increased silent refluxes. In careful Valsalva maneuvering, I spontaneously breathe very little but inhale via the right eardrum – what does that say about the Eustachian tube’s functionality?
This indicate dysfunctions probably associated with the Osteomeatal Complex, which has complex interacting functions, where one can be associated with “.. duration of nasopharyngeal pressure phase during Toynbee maneuver … influencing middle ear pressure .. can be measured “by sonotubometry, tympanometry and nasopharynx manometry”. https://pubmed.ncbi.nlm.nih.gov/11189424/
“The Toynbee maneuver, swallowing when the nose is obstructed, leads in most cases to pressure changes in one or both middle ears, resulting in a sensation of fullness. … “New information concerning the rapid pressure variations in the nasopharynx and middle ear during deglutition with an obstructed nose was obtained. Typical individual nasopharyngeal pressure change patterns were recorded, ranging from a maximal positive pressure of +450 to a negative pressure as low as -320 mm H2O”. https://pubmed.ncbi.nlm.nih.gov/3355049/ Sometimes, ”retracted, closed nose” when waking up at night (see also Locus Coeruleus above), indicating change between positive and negative pressure?
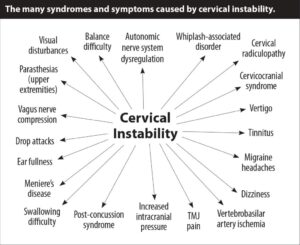
G: Spinal dysfunction, here preferably cervical and lumbal, is often discussed as (part of or completely) tinnitus. Refer to the introduction link above. Here only a picture that cover an overview. Some of the arrows interplay in complex ways – so, if tinnitus is one arrow, this do not cover the multidisciplinary/ multifaceted story.
https://www.caringmedical.com/prolotherapy-news/tinnitus
More ..
Trigeminovascular System (see pathways) https://www.sciencedirect.com/topics/neuroscience/trigeminovascular-system
Tear (not emotional!) “small flow” activated during e.g. massage of the spine and night up waking. https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-018-0843-5/figures/4
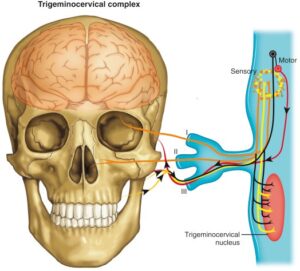
The trigeminocervical complex
(https://books.google.se/books?id=xjtRDwAAQBAJ&pg=PA184&lpg=PA184&dq=teeth,+oral+mucosa,+and+the+greater+occipital+nerve,+which+may+account+for+the+migraine+triggers+emanating+from+the+neck&source=bl&ots=fSxfbH-4Nl&sig=ACfU3U3lkThe4ht5do-VjGr3B5fkJHm6DQ&hl=en&sa=X&ved=2ahUKEwiZ5MKut6L4AhW5Q_EDHS-4AdkQ6AF6BAgCEAM#v=onepage&q=teeth%2C%20oral%20mucosa%2C%20and%20the%20greater%20occipital%20nerve%2C%20which%20may%20account%20for%20the%20migraine%20triggers%20emanating%20from%20the%20neck&f=false)
mediates the pain and symptoms of migraine.19–21 The trigeminocervical complex is formed in part by the trigeminal caudal nucleus, and extends from the level of dorsal spinal horn up to the trigeminal nerve distribution in the face and down to C1and C2 (Fig. 2).21 Stimulation of the superior sagittal sinus, dura mater, and cerebral vessels all in turn trigger the trigeminocervical complex.21 This complex also receives afferent stimuli converging from the face, teeth, oral mucosa, and the greater occipital nerve, which may account for the migraine triggers emanating from the neck and temporomandibular joint musculature.21
Fig. 2. The trigeminocervical complex.
In a “sinus-like” presentation of migraine, pain can be perceived in the maxillary and ophthalmic regions of the trigeminocervical complex, also causing pain and pressure to be felt in and/or around the eyes and sinuses. Sensitization of the trigeminocervical network can in turn cause nasal congestion with rhinorrhea, itchy nose, periorbital swelling, and lacrimation via stimulation of the parasympathetic fibers during an active migraine.19,21 Neurologic signs from this heightened parasympathetic stimulation to the head are found during migraine exacerbations in 73% of migraineurs, and are often bilateral.22
Spinal stenosis can influence the Trigeminalcervikal complex
https://www.mayoclinic.org/diseases-conditions/spinal-stenosis/symptoms-causes/syc-20352961 Spinal stenosis is a narrowing of the spaces within your spine, which can put pressure on the nerves that travel through the spine. Spinal stenosis occurs most often in the lower back and the neck.
Some people with spinal stenosis may not have symptoms. Others may experience pain, tingling, numbness and muscle weakness. Symptoms can worsen over time.
Spinal stenosis is most commonly caused by wear-and-tear changes in the spine related to osteoarthritis. In severe cases of spinal stenosis, doctors may recommend surgery to create additional space for the spinal cord or nerves.”
But also, surprising .. Tympanic Resonance Hypothesis
https://www.frontiersin.org/articles/10.3389/fneur.2020.00014/full
“Seemingly unrelated symptoms in the head and neck region are eliminated when a patch is applied on specific locations on the Tympanic Membrane. Clinically, two distinct patient populations can be distinguished; cervical and masticatory muscle tensions are involved, and mental moods of anxiety or need. Clinical observations lead to the hypothesis of a “Tympanic Resonance Regulating System.” Its controller, the Trigeminocervical complex*, integrates external auditory, somatosensory, and central impulses. It modulates auditory attention, and directs it toward unpredictable external or expected domestic and internal sounds: peripherally by shifting the resonance frequencies of the Tympanic Membrane; centrally by influencing the throughput of auditory information to the neural attention networks that toggle between scanning and focusing; and thus altering the perception of auditory information. The hypothesis leads to the assumption that the Trigeminocervical complex is composed of a dorsal component, and a ventral one which may overlap with the concept of “Trigeminovagal complex.” “Tympanic Dissonance” results in a host of local and distant symptoms, most of which can be attributed to activation of the Trigeminocervical complex. Diagnostic and therapeutic measures for this “Tympanic Dissonance Syndrome” are suggested.”
* The convergent inputs to the central projection of the trigeminovascular system, the trigeminal nucleus caudalis and the C1 and C2 regions of the spinal cord, collectively known as the trigeminocervical complex (TCC) is thought to explain the common distribution of pain in migraine. https://www.medscape.com/viewarticle/812123 NB include? Silent Migraine?
Also to be considered?
https://www.sciencedirect.com/topics/medicine-and-dentistry/caudal-trigeminal-nucleus
H: The interplay between and “Reciprocal Causal Relationship between Laryngopharyngeal Reflux and Eustachian Tube Obstruction” https://medcraveonline.com/JOENTR/reciprocal-causal-relationship-between-laryngopharyngeal-reflux-and-eustachian-tube-obstruction.html is very complex and not well understood yet. With Valsalva maneuver we can some information, but not all of course.
I use a quite much modified Valsalva Maneuver (careful blowing in and out when holding your nose for trying to find out how such complex processes can be part of my problems. “My Valsalva way” reveal that e.g. I can breathe in from my right ear but also that indicate some problems in my nose at middle nasal concha. A question I have is: Can such interplay (title above) in some way also influence my 60-years old tinnitus (audiogram at https://carism.se/2021-22/personal-clinical-situation/)
Some more about – “The Valsalva maneuver with otoscopic visualization of the excursion of the eardrum is the most reliable test of tubal function. Tympanometry is used mainly for documentation”. https://pubmed.ncbi.nlm.nih.gov/2386456/
“Use the Valsalva maneuver – This simple trick helps open your Eustachian tube. To perform this maneuver, take a deep breath and pinch your nose. With your mouth closed, attempt to exhale gently through your nose. This should create enough pressure to “pop” or unclog the ear. Don’t blow too hard to avoid damaging your eardrum. Once your Eustachian tube opens, chew gum or suck on hard candy to keep it opened.” https://www.healthline.com/health/why-does-my-ear-feel-clogged#treatments
“My way” is to combine (not at the very same time) Valsalva and Toynbee strategies and thereby achieve some decrease in the increasing hard sounds during sleep when I am awakened by such very hard increase. Also, may my well-trained breathing strategies influence increased LC, which is thought of in some cases over react when “started again” after REM-sleep.
More links – Eustachian Tube Function – https://www.ncbi.nlm.nih.gov/books/NBK532284/
I: Coming
Synopsis (coming)